
On Jan. 8, 1929, Dr. L.E. Bensom of Los Angeles used his vacation to mush to native villages in Alaska. At the close of a particularly hard day on the trail, he found himself with 70 patients on his hands, all suffering from smallpox. There were 100 people in the village with no medical facilities.
Vaccines delivered by drones and by burros. People who shout about the danger of vaccines and refuse to get a jab. Public health campaigns to convince the vaccine hesitant. Public criticism of a failure to provide vaccines for lower-income countries and marginalized populations.
These are all part of the unprecedented world vaccination campaign now going on.
They're also the hot-button topics that go back to the very first vaccine — for smallpox in 1796.

Doctor Sergen Saracoglu (left) and nurse Yilzdiz Ayten (center) from the Bahcesaray Public Hospital vaccination team, arrive at the village of Guneyyamac in eastern Turkey on Feb. 15, 2021, as part of an expedition to vaccinate residents 65 years and over with Sinovac's CoronaVac COVID-19 vaccine.
In photographs and illustrations from past and present vaccine campaigns, you can see both the similarities and the striking contrasts.
James Colgrove, a professor of sociomedical sciences at Columbia University, and Sanjoy Bhattacharya, a professor of history at the University of York and director of the WHO Collaborating Center for Global Health Histories, helped us out with historical context to go along with the images.
The vaccine has been created! Now ... how to get it where it needs to go?
Getting a vaccine from point A to point B has been a logistical problem since the very start with the smallpox vaccines, says Bhattacharya.
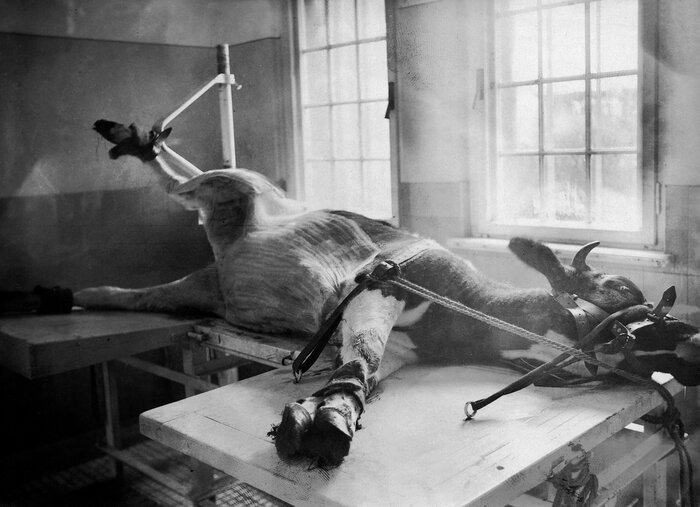
On Jan. 1, 1900, a young cow is tied onto a table waiting for the extraction of pox sore to be used for vaccines for smallpox.
The solution? Medical teams would take children (in one case, orphans were used to transport the virus from Spain to its colonies) and animals (like cows and horses) from village to village or from country to country, harvesting liquid from smallpox or cowpox sores and getting it under the skin of an unvaccinated person. But that was clearly not a sustainable practice, says Bhattacharya, for ethical and scientific reasons.
Many years of innovation later followed, including the development of freeze-dried vaccines. The COVID vaccine world is currently dependent on cold chain technology that uses super freezers to keep vaccines at temperatures as low as -13 degrees Fahrenheit while they make their way on planes, trains and automobiles.

Ousseynou Badiane, head of Senegal's vaccination program, stands in front of newly built cold rooms at Fann Hospital in Dakar on Jan. 22, 2021. These cold rooms may be used to help store the country's stock of COVID-19 vaccines.
Relying on cold storage technology is still not a perfect system.
The challenge has always been the greatest in poor and rural areas. "You have to make sure you have generators to maintain refrigerators," says Colgrove. It is the same problem countries are having with the COVID vaccine today.

Left: A West German Navy vessel hands over vaccines to the U.S. transport General Patch in July 1957 for 134 people sick with the Asiatic flu. The ship was anchored 20 miles off Bremerhaven, West Germany, after being quarantined for a flu outbreak. Right: Health workers in a speed boat on their way to vaccinate Quilombo communities against COVID-19 in Oriximina, Brazil in Feb. 2021.
Vaccine inequity is "just one part of a larger picture of inequity," says Colgrove. "People have been unvaccinated for the same set of reasons that they have always been deprived of other material goods."
For every vaccine, there's been a campaign against it.
"Anti-vaccination movements are as old as vaccines themselves," says Bhattacharya.
What drives people to oppose a vaccine? You have to look at what is happening in a country or community culturally and politically and that is where you'll find your answers. It is usually a combination of factors that create doubts about how safe and effective a vaccine is, says Bhattacharya.
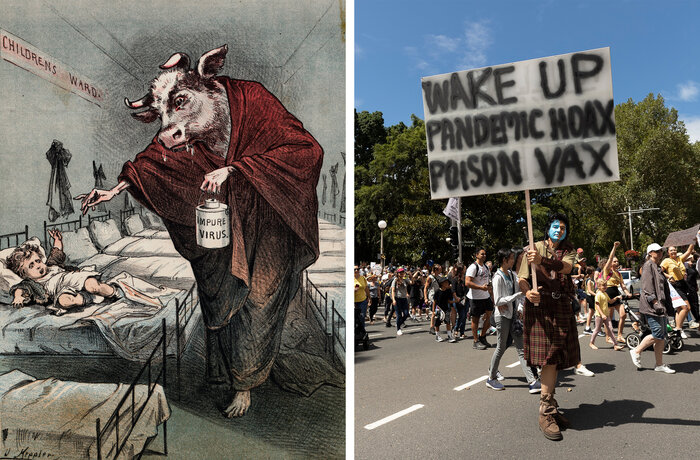
Left: A drawing of a human with a cow head holding a needle menacingly toward a young child as he administers a tainted smallpox vaccination is meant to sow distrust of smallpox vaccines. Right: Protesters against mandatory COVID-19 vaccinations at a rally in Sydney on Feb. 20, 2021.
But what really gets people riled up, says Colgrove, is when governments mandate vaccinations. "What gets people marching in the stress, forming orgs, creating pamphlets is when governments start to require it. If you don't want the vaccine but you don't feel like anyone is forcing you to get it, then you just don't get it. Antivaccination movements really arose in the mid-19th century when governments started to require it."
There have always been trust issues.
A vaccine campaign must address the issues of trust between those giving the vaccines and those receiving it, says Bhattacharya. You can't run it just with logistics. The vaccine campaigns that don't take trust into account end up struggling while the process drags on to get a disease under control.
In the case of polio, says Bhattacharya, it was difficult to convince communities to get the vaccine in places where governments hadn't acted in the communities' interest on other issues.

Boys stand in line to be vaccinated through the Smallpox Eradication and Measles Control Program run by USAID and the Communicable Disease Center in West Africa in 1968. While smallpox has been eradicated, measles is still one of the leading causes of death among young children, even though a safe and cost-effective vaccine is available, reports the World Health Organization.

People wait to see if they get a reaction after receiving their COVID-19 vaccines at a vaccination center at Salisbury Cathedral on Feb. 11, 2021 in Salisbury, England.
"It was about [the government] convincing people that the polio vaccination was about their best interests in a context where governments had done little for their general welfare. This was the context in which polio vaccination drives were resisted in Northern India, for example," says Bhattacharya. People have said it was superstition about the vaccine that prevented Indians from getting the vaccine, but it was actually about "a fundamental lack of trust."
It's all about the advertising.
To get the word out and make a convincing argument about the vaccine, it's all about marketing and messaging. Advertising techniques were first used in the 1920s for diphtheria immunizations, says Colgrove (think images of smiling babies with warnings in red ink that diphtheria kills).
The way a vaccine is given is also critical. The first oral vaccine in the 1960s for polio replaced the hypodermic needle. It certainly made it a much easier sell to those who might be hesitant or fearful of the actual process using needles, says Colgrove.
"Needle phobia is a big deal and orally administered vaccines are more acceptable to many people. Also you don't have to worry about the injection equipment [which was helpful for mass vaccinations]," says Colgrove. "In fact one of the reasons the global polio eradication ended up being so successful was they used the oral vaccine as opposed to the injected vaccine." The oral vaccine also did a better job of protecting against the virus.
The West makes the vaccines and the rules. That's actually kinda new.
The West wasn't always the main player in vaccine production — although it was always on the path to be. Following World War II, several newly independent (decolonized) countries were keen to develop their own vaccine production capabilities. Two examples are India and Pakistan, says Bhattacharya.
"Countries like India and Pakistan were able to play Cold War foes [U.S. and USSR] against each other to get access to new vaccine production technologies, assistance in setting up new vaccine production units," he adds.
So how did the West ultimately get control? In that post-World War II era in the West, people started to realize there was money to be made in all pharmaceuticals (not just vaccines) and "the business landscape changed," says Colgrove.

Marie Josette Francou (right), a Red Cross nurse, vaccinates a child against cholera on Oct. 10, 1953 in Mong Duc, Indochina (now known as Vietnam).
What had been a cottage industry of small pharmaceutical companies, individual investigators and physician scientists started producing more products along with vaccines, says Colgrove. They evolved into the mega companies that exist today.
That said, other countries are still in the vaccination business — albeit with mixed results — including Russia's Sputnik V, China's Sinovac and outlier Cuba.

Workers wait to open the secure door in the packaging area of Sinopharm COVID-19 vaccine during a media tour organized by the State Council Information Office on Feb. 26, 2021 in Beijing, China. Sinopharm, one of China's largest state-owned biotech companies, says it is able to ramp up production to one billion doses in 2021.
The power and politics behind vaccines.
Politicians love their mottos and the vaccination effort is no different. In the U.S., government officials called it Operation Warp Speed and now the "We Can Do This" campaign. In Germany it's "Vaccinate, Vaccinate Vaccinate." In Israel it's "Getting Back To Life."
So, how much of vaccine production and distribution is about political power and money?
Bhattacharya says pretty much all of it. "Pandemic responses, including the vaccination programs that underpin them, are always political. Those who claim that they know the means of accentuating 'global solidarity' are no less political; they just have different political goals."

Left: Thousands of New Yorkers, on an appeal by government officials, came to city hospitals and health stations to get vaccinated against smallpox. This is a shot of the line outside Morrisania Hospital in the Bronx on April 14, 1947. Right: In this aerial view from a drone, cars line up for a mass COVID-19 vaccination event on Jan. 30, 2021 in Denver.
And the money? Most vaccines wouldn't exist if Big Pharma didn't make a profit off of them, says Colgrove.
One of the criticisms is that we have vaccines for diseases that burden rich countries but not for those diseases that plague poor countries — like malaria and dengue fever. "If those diseases were a problem in Europe and the U.S. we would probably have vaccines for them now."
That's the contradiction of the pharma industry, says Colgrove. "On the one hand they produce these drugs for the benefit of everyone but their mission is to make profits for their shareholders."
What will the world say about the COVID-19 vaccination effort in 100 years?
People will not remember the details, says Colgrove. Take, for example, the polio vaccine rollout, he says. If you ask the average person today, they would say it was a huge success, but people forget it was total chaos for a while.
"There were a lot of problems with the initial distribution during the period when the demand exceeded the supply. The polio vaccine was developed by a nonprofit foundation. The U.S. government had very little involvement because the Eisenhower administration saw involvement as the opening for socialized medicine.
"There was also lots of confusion and uncertainty about who should get the vaccine first and supplies were limited. There were stories of rich people pulling strings to get their kids vaccinated first."

Sanitation worker Ramesh Solanki cleans the streets outside Palghar railway station. "I get up every morning at 5:30, and I see news about the vaccines on TV," he says. "I don't know about any controversies. I just know I'm proud to be part of this." As a sanitation worker, he's among the first Indians eligible to get the coronavirus vaccine.
When it came to the COVID vaccine, the CDC knew there were limited supplies so they were able to prioritize certain populations [healthcare workers, the elderly] says Colgrove. "But I think the way people will remember the COVID rollout will depend on what happens in the coming months and years."
No one can deny the incredible feat of making vaccines in a year. But Bhattacharya points to another legacy.
Bhattacharya says it's unfortunate, but this vaccination effort will be all about profits, not humanity — the world was let down when it comes to equity and access to the vaccine.

Two men, wearing personal protective equipment, visit the grave of a relative at Pondok Rangon public cemetery, reserved for suspected COVID-19 victims, on Dec. 24, 2020 in Jakarta, Indonesia.
"I think our descendants will look back with some shame at the efforts of so many private vaccine producers to make immense profit from human misery and anxiety."


No comments:
Post a Comment