Related online courses
The Role of Physical Activity in Specific Conditions – PhysioplusThe Role of Physical Activity in Specific Conditions Who will benefit from Physical Activity? Sign Up I am grateful to you, Physiopedia and all your partners who contributed to make this very disabling but yet completely treatable condition come to us. This will indeed result in increased availability of treatment centers around the world, thus reducing the effect of this condition. See more testimonials Introduction Physical activity plays an important part in the health and wellbeing of people with different conditions. These conditions could be short or long term and it is important for the physiotherapists to know the benefits and when and how to prescribe physical activity. This course explores the role of physical activity in long term or age related conditions and explores conditions that may only be temporary such as pre and post surgery and pregnancy. Aims This course will cover physical activity benefits, contraindications and prescription in different short term and long term conditions. Outline This course is made up of videos, reading, discussions and a final quiz. The course content is split into the following sections: Physical activity with pre and post surgery and acute care Physical activity in pregnancy Physical activity with increased age Physical activity in long term musculoskeletal conditions Physical activity in neurological conditions Physical activity in HIV/AIDS Target audience This course is aimed at Physiotherapy and Physical Therapy clinicians, students and assistants. Other interested professionals such as athletic trainers, occupational therapists, nurses or medical doctors interested in this subject are also invited to participate. More details Practicalities Hours of Learning - No deadlines are applied to this course and it can be started and completed in your own time according to your personal schedule. We expect the required elements to take around 4 - 4.5 hours depending on your schedule and learning style. Additionally there are many optional resources provided and if you choose to review these the course could take longer to complete. Types of Activities - Reading Physiopedia pages, journal articles, book chapters. Watching videos. Attempting quizzes. Participating in an international discussion forum. Certificates - At the end of the course, when you have completed all of the required elements, you will be able to download a certificate of completion and 4.2 Physioplus points will be added to your personalised learning dashboard. Requirements to complete this course In order to complete this course and receive a course completion certificate plus CEUs/CCUs/CPD points you will need to: Respect the Physioplus Community Culture. Log all the required learning activities as complete (represented by the orange icons!). Actively and appropriately participate in the course discussions. Pass a final quiz with a score of 80% or more. Complete a course evaluation form. Learning outcomes At the end of this course you will be able to: describe at least 2 benefits of physical activity in relation to the specific conditions listed in this course list at least 2 contraindications for physical activity in acute care, pregnancy, and the elderly plan a physical activity program based upon case representations for patients with specific conditions Presented by: Physioplus Team A team of committed individuals with a very wide variety of clinical and educational experience. View all courses by Physioplus Team certificate of completion 4.2 Physioplus points Accredited by 3 organisations Related courses • Definition/Description
The Centers for Disease Control and Prevention (CDC) revised the definition of AIDS in 1992 to include those who have HIV-1 and a CD4 count below 200/mL (the normal CD4 lymphocyte count is 600 to 1200/mL) or 14% of the total lymphocyte count, even if the person has no other signs or symptoms of infection. Three distinct points identify this continuum:
- Asymptomatic HIV seropositive,
- Early symptomatic HIV, and
- HIV advanced disease (AIDS).[1]
AIDS, acquired immunodeficiency syndrome, is a contagious, chronic and life-threatening condition caused by the human immunodeficiency virus (HIV). Acquired means the disease is not inherited or genetic in nature but develops as a result of a virus. Immuno refers to the immune system, and deficiency means the immune system is underperforming or hypoactive. By damaging your immune system, HIV interferes with your body's ability to fight off viruses, bacteria, and fungi that cause disease and other invasive pathologies. HIV makes you more susceptible to certain types of cancers and infections your body would normally resist. The cytopathogenic virus and the infection itself are known as HIV. "Acquired immunodeficiency syndrome (AIDS)" is the name given to the later and more serious stages of an HIV infection. [2]
According the AIDS.gov, 35.3 million people are currently living with HIV/AIDS worldwide. Though the spread of the virus has slowed in some countries, it has escalated or remained unchanged in others. The best hope for stemming the spread of HIV lies in prevention, treatment and education. [3]
For a visual illustration of how HIV and AIDs progresses, please visit this weblink
Prevalence
Prevalence is defined as the number of people living with HIV infection at the end of a given year. In 2018 it is estimated that approximately 37.9 million people worldwide are living with HIV. 36.2 million adults and 1.7 million children (<15 years). with the number of new infections being around 1.7million.
[4] According to the CDC, at the end of 2016, about 1.1 million people in the United States were living with HIV/AIDS. Of those people, about 14% do not know they are infected. The prevalence of HIV is increased in African American males, male to male sexual relations, and age 25-34. The prevalence is 5 times greater in incarcerated populations than the general population at large. The high HIV transmission rates among inmates maybe related to homosexual encounters and potentially tattooing. Ethnicity is not directly related to AIDS risk, but it is associated with other determinants of health status such as poverty, illegal drug use, access to health care, and living in communities with a high prevalence of AIDS.
[5]Incidence is the number of new HIV infections that occur during a given year. HIV infection is the 5th leading cause of death for people who are between the ages of 25-44 years old in the United States. In 2018, the CDC estimated that approximately 37,832 people were newly infected with HIV
[4]. There are four transmission categories of HIV: male to male sexual relations, heterosexual relations, injection drug users, and homosexual relations combined with injection drug users. Male to male sex accounted for 69% of new HIV infections, hetrosexuals 24% of all new infections in 2018. Furthermore, black men represented 42% of all new HIV infections, in the United States, in 2018. Black/African American men and women were also strongly affected and were estimated to have an incidence rate that was higher than the incidence rate among whites. African-American's represent about 14% of the total United States population, but make up almost half of the people known that are suffering from AIDS. AIDS is the leading cause of death for African-American men between the ages of 35-44 years old in the United States.
[5]For complete HIV/AIDS prevalence and incidence statistics, please visit
CDC factsheet or visit the
HIV/AIDS page on the CDC.
Clinical Presentation
The clinical presentation of HIV and AIDS vary depending on which stage of infection the person is in.
Early Infection
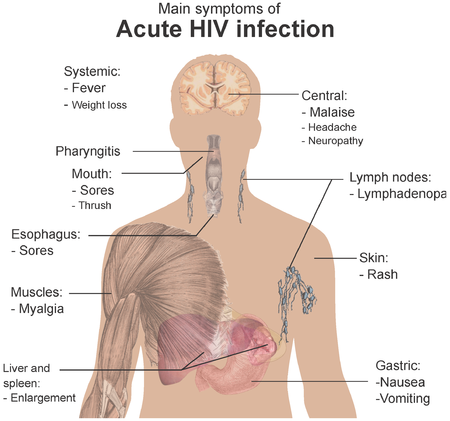
When a person first becomes infected with HIV, many people will experience flu-like symptoms often described as "the worst flu ever." These symptoms usually occur within 2-4 weeks of becoming infected with HIV. Early signs and symptoms may include: fever, headache, sore throat, swollen lymph vessels, fatigue, muscle and joint aches and pain, and rash. GI complaints include change in bowel and bladder function, especially diarrhea. Cutaneous complaints are common and include: dry skin, new skin rashes, and nail bed changes. Because these are very common and present in a number of other diseases, a combination of complaints is more suggestive of HIV infection than any one sign/symptom. In addition, many people with HIV present with back pain, but the underlying cause may differ from person to person. Back pain may be due to: muscle weakness and atrophy that occurs as a result of the disease process. Back muscle weakness and atrophy can alter the person's normal postural alignment and may cause subsequent back pain as well as a person's response to their medications may contribute to back pain as well. It has been reported that back pain is more likely to occur when the bodies T-cell count drops. Even though, the person may or may not exhibit symptoms they can still transmit the virus to others. Once, the virus enters the person's body, the person's immune system comes under attack. The virus then starts to multiply in the person's lymph nodes and slowly begins to eradicate the helper T- cells, the white blood cells that help the immune system. [3] [5] [2]
Later Infection
A person may remain symptom free for as long as 8-9 years, but as the virus continues to multiply and destroy immune cells, the person may begin to develop chronic symptoms and/or acquire mild infections. Chronic symptoms seen in this stage are but not limited to the following: swollen lymph nodes-which is often one of the first signs of HIV infection, diarrhea, weight loss, fever, cough and shortness of breath. [3]
Latest Phase of Infection
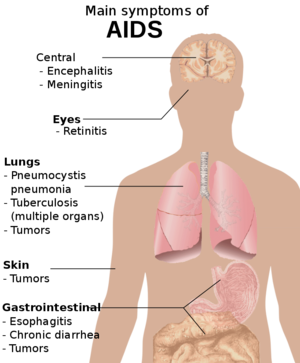
Usually, after a person has been infected with HIV for 10 years or more the last phase of HIV commences. More serious symptoms of the virus start to appear and the infection may then meet the official definition of AIDS. Some of the signs/symptoms of later infection are: Kaposi's sarcoma, multiple purple blotches and bumps on skin, HTN (pulmonary and or cardiac), dyspnea, syncope, chest pain, non-productive cough, easy bruising, thrush, muscle atrophy and weakness, back pain, poor wound healing, HIV related dementia (memory loss, confusion, behavioral change, impaired gait), and distal symmetric polyneuropathy (pain, numbness, tingling, burning, weakness, and atrophy). By the time AIDS develops, the person's immune system has been severely damaged, making the person susceptible to many opportunistic infections such as TB, Pneumocystsis carinii, pneumonia, lymphoma, thrush, herpes 1 and 2, toxoplasmosis and cansisiasis. They are called "opportunistic" infections or diseases because they take advantage of the compromised immune system to infect and destroy the person's body. Under normal conditions, a person would not be affected to the degree of severity they are under the presence of these infections with normal immune function. The signs and symptoms of some of these infections may include but not limited to the following: soaking night sweats, shaking chills or fever higher than 100 degrees F (38 C) for several weeks, dry cough and shortness of breath, chronic diarrhea, persistent white spots or unusual lesions on the person's tongue or in their mouth, headaches, blurred and distorted vision, weight loss. [2]
In 1993, the CDC redefined AIDS to mean the presence of HIV infection as shown by a positive HIV antibody test with the presence of at least one of the following: [3]
- If an individual has HIV and one or more of certain opportunistic infections (OIs) defined by the CDC no matter what that person's CD4 count is. The CDC lists more than 20 OIs that are considered AIDS-defining conditions. These are:
- Candidiasis of bronchi, trachea, esophagus, or lungs
- Invasive cervical cancer
- Coccidioidomycosis
- Cryptococcosis
- Cryptosporidiosis, chronic intestinal (greater than 1 month's duration)
- Cytomegalovirus disease (particularly CMV retinitis)
- Encephalopathy, HIV-related
- Herpes simplex: chronic ulcer(s) (greater than 1 month's duration); or bronchitis, pneumonitis, or esophagitis
- Histoplasmosis
- Isosporiasis, chronic intestinal (greater than 1 month's duration)
- Kaposi's sarcomav
- Lymphoma, multiple forms
- Mycobacterium avium complex
- Tuberculosis
- Pneumocystis carinii pneumonia
- Pneumonia, recurrent
- Progressive multifocal leukoencephalopathy
- Salmonella septicemia, recurrent
- Toxoplasmosis of brain
- Wasting syndrome due to HIV
- A CD4 lymphocyte, helper T cell count of 200 or less. According to AIDS.gov recent research has shown that it may be easier to mainatin higher CD4 counts if you start treatment before your count drops below 350. Normal count ranges from 500 to 1,000.
- Certain Cancers such as: Lymphoma, CNS Lymphoma, Kaposi's Sarcoma, Anal Cancer, and Invasive Cervical Cancer.
Associated Co-morbidities
AIDS is an unique disease in that no other known infectious disease attacks the immune system directly in the same manner. Because the immune system is greatly affected many patient's suffering from AIDS may present with the folllowing co-morbidities among others:[6][7]
- Cancer (especially with the appearance of the highly unusual Kaposi's Sarcoma)
- Non-Hodgkin's Lymphoma
- AIDS-related primary central nervous system lymphoma
- Hepatocellular carcinoma
- Tuberculosis (pulmonary and extrapulmonary TB)
- HIV neurologic disease
- AIDS dementia complex/HIV encephalopathy
- Progressive multifocal leukoencephalopathy
- Vacuolar myelopathy (most common in the Thoracic spine)
- Inflammatory polyneuropathies
- Sensory neuropathies
- Mononeuropathies
- Inflammatory demylinating polyneuropathy (similar to Guillain-Barre syndrome)
- Cytomegalovirus
- Hypersensitivity disorders
- A twofold increase in risk of Myocardial Infarction[8]
- Chronic Kidney Failure [8]
- Osteoporosis [8]
Medications
When HIV was first identified there were few drugs to treat the virus and opportunistic infections associated with it. Since then, a number of medications have been developed to treat both HIV/AIDS and opportunistic infections. Anti-retroviral medications have provided HIV-positive Americans with an increased quality of life and extended life. No drug/treatment can cure HIV/AIDS, many of the drugs used have side effects that can be severe, and most drug therapies are expensive.
Anti-retroviral drugs inhibit the growth and replication of HIV at various stages of its life cycle. Seven classes of these drugs are available:
- Nucleoside analogue reverse transcriptase/NRTIs
- Protease inhibitors/PIs
- Non-nucleoside reverse trabscriptase inhibitors/NNRTIs
- Nucleotide reverse transcriptase inhibitors/NtRTIs
- Fusion inhibitors
- Integrase inhibitors
- Chemokine co-receptor inhibitors
To learn more about how these anti-retroviral drugs prevent HIV from replicating in your body, visit http://aids.gov/hiv-aids-basics/just-diagnosed-with-hiv-aids/treatment-options/overview-of-hiv-treatments/index.html
A person's response to any of these medications is measured by viral load. Viral load is tested at the start of any treatment and then every three to four months while undergoing therapy.
Taking more than one drug protects the patient against HIV-drug resistance. Taking 3 different HIV medications does the best job of controlling the amount of virus in your body and protecting the immune system. Therefore, by following the 3-drug regimen, HIV will be less likely to reproduce and not respond to the medications. [3]
Side Effects of Medication
Short Term:
- Rash
- Anaemia
- Diarrhoea
- Nausea
- Headaches
- Dizziness
- Muscle pain
- Weakness
- Fatigue
- Insomnia
Long Term:
- Lipodystrophy- a problem in the way the body produces, uses, and stores fat
- Insulin Resistance
- Lipid Abnormalities
- Decrease in bone density
- Lactic Acidosis
Hepatotoxicity is also a common complication which may manifest itself with the following signs/symptoms:
- Carpal tunnel syndrome
- Palmar erythema (also known as Liver palms) - reddening in bothe palms
- Asterixis - a tremor in the hand when the wrist is extended
- Signs of liver impairment
If the patient notices any unusual or severe reactions after starting or changing a drug, report the side-effects to your health care provider immediately. Do not let these side-effects take over the patients treatment plan. [3]
For complete description of HIV drugs, including brand names, see AIDSmeds.com's Treatment for HIV and AIDS. [9]
Diagnostic Tests
Early diagnosis is important so that early preventative therapies may be initiated, and sex partners can be notified of their risk of HIV. The U.S. Food and Drug Administration approved the first rapid HIV test in August 2013. This new test allows for simultaneous detection of HIV-1 p24 antigen as well as antibodies to HIV-1 and HIV-2 in human serum, plasma, and venous or fingerstick whole blood specimens. The Alere Determine HIV-1/2 Ag/Ab Combo test is the first FDA-approved test which independently distinguishes results for HIV-1 p24 antigen and HIV antibodies in a single test. Detection of HIV-1 antigen permits earlier detection of HIV-1 infection than is possible by testing for HIV-1 antibodies alone. The test can distinguish acute HIV-1 infection from established HIV-1 infection when the blood specimen is positive for HIV-1 p24 antigen but is negative for HIV-1 and HIV-2 antibodies
“This test helps diagnose HIV infection at an earlier time in outreach settings, allowing individuals to seek medical care sooner,” Karen Midthun, M.D., director of the FDA’s Center for Biologics Evaluation and Research. [3]
Other methods of screening for AIDS can be done by a finger stick blood test, the HIV-1 antibody enzyme immunoassay test. The blood test looks for the presence of antibodies to HIV-1. The test only indicates if person has been exposed to the virus. Antibody testing is not always reliable because the body takes varying amounts of time to produce a detectable level of antibodies. Consequently, a person who does have HIV could test negative for the for HIV antibodies. Antibody testing is also unreliable in neonates because transferred maternal antibodies are present for 6-10 months in the neonate. The Western blot test can be used when there is concern about false-positive results. HIV RNA viral loading is another test that can be done in the lab. It measures the plasma HIV RNA assay. OraQuick Rapid HIV Antibody Test is another test which individuals may use. This test is quick and results are available in 20 minutes. The test is a rapid, non-invasive test which uses saliva or a gum swab to detect the presence of HIV antibodies. The advantages to rapid testing is individuals with positive results can receive treatment quickly and education about how to prevent transmission of the illness to others and can partake in counseling nded. The disadvantage of this quick test is it cannot detect the HIV infection in people who were exposed less than 3 months prior to taking the test. It has been estimated that one third of all individuals who do get tested for the presence hand we of HIV do not return to get the results of their test.[5]
Causes
Around the late 1970's and 80's doctors began noticing that an increasing number of people were suffering from several unusual and rare illnesses. At first, little was known about what was happening to these initial victims of AIDS. Doctors were unsure as to what was causing the condition. Many of the first people diagnosed with this new condition were homosexual men. Due to the infected population, the condition was labeled GRID, gay related immunodeficiency. However, the condition soon started showing up in women, intravenous drug users, and hemophiliacs. The first reported AIDS cases were in the United states in 1981. In 1983, the Institute Pasteur in France regonized the virus which was causing so much panic was the result of AIDS. The virus that resulted from AIDS was named HIV, human immunodeficiency virus. Researchers in France, now understood the virus passed from each person via the exchange of semen, blood, or vaginal secretions during sexual contact. Researchers also learned that AIDS weakens the immune system by destroying the body's white blood cells, specifically the helper T-cells. Helper T- cells help the body fight off viruses and bacteria that enter the body. In 1985 another breakthrough took place, a blood test which detected the presence of HIV antibodies in the person's blood stream. The first sample of HIV infected blood dates back to 1959, but computer analysis dates the emergence date back to the 1930's.
There have been many theories and much speculation as to where the AIDS virus first originated. AIDS used to be a very rare and isolated virus which affected a few types of monkeys and chimpanzees in Africa. AIDS is related to another virus, Simian Immunodeficiency virus that affects monkeys and apes. It was thought that humans were first exposed to AIDS when they caught the monkeys for food, kept them as pets, or if they were scratched and bitten by an infected monkey/ape.
We now know that AIDS is caused by the spread of the HIV virus. The virus is spread though sexual contact; needles; a syringe that is shared by intravenous drug users; transfusion of infected blood or blood products; or perinatal transmission from infected birthing or breastfeeding a child from an infected mother. HIV is not transmitted through casual contact such as: the shared use of utensils, food, cups, towels, razors, toothbrushes or even kissing. Transmission always involves exposure to some body fluid from an infected client. The greatest concentrations of the virus have been found in blood, semen, cerebrospinal fluid, and cervical/vaginal secretions. HIV has been found to be in low concentrations in tears, saliva, and urine, but no cases of transmission have been reported via these routes. The primary cause of AIDS is the type 1 retrovirus, or HIV. Transmission of the HIV virus happens by individuals partaking in high risk behaviors. High risk behaviors are defined and include: unprotected vaginal, anal, or oral sex; having 6 or more sexual partners in the past year; sexual activity with someone known to carry HIV; exchanging sex for money or drugs; and injecting drugs.
Population groups at the greatest risk are: commercial sex workers (prostitutes) and their clients; homosexual men; injection drug users; blood recipients; dialysis recipients; organ transplant recipients; fetuses of HIV infected mothers; and people with other sexually transmitted diseases. People who already have a sexually transmitted disease are 3-5 times more likely to come in to contact with the HIV virus compared with people without STDs. [5][2]
Systemic Involvement
HIV is described mainly as a infection of the immune system resulting in progressive and profound immune suppression. The progression of the illness can have an effect on the following systems: musculoskeletal, neurologic/neuromuscular, cardiopulmonary, and the integumentary system. Some of the clinical manifestations of HIV on the musculoskeletal system is but not limited to:
- Myalgia/arthralgia
- Rheumatologic manifestations
- Inflamed joints and associated disorders like:
HIV can have the following implications on the neurologic/neuromuscular system:
- Gait disturbances
- Intention tremor
- Delayed response of reflexes
- HIV associated dementia
- Socially withdrawn
- Irritability
- Depression
- Apathy
- Lethargy
- Memory impairment
- Confusion
- Disorientation
- Ataxia
- Leg weakness with gait disturbances
- Loss of fine motor coordination
- Incontinence
- Paraplegia
- Guillain-Barre syndrome
- Headaches
- Seizures
- Radiculopathy
- Peripheral neuropathy
- Brachial neuropathy
- Vacuolar spinal myelopathy
The cardiopulmonary system can display the following clinical signs/symptoms:
- Dyspnea, especially on exertion
- Nonproductive cough
- Hypoxia symptoms
- Pericardial effusion
- Cardiomyopathy
- Endocarditis
- Vasculitis
The integumentary system can display the following clinical manifestations:
- Hair loss
- Basal cell carcinoma
- Kaposi's sarcoma
- Mucocutaneous ulcers
- Rashes
- Urticaria
- Delayed wound healing [6][7]
Medical Management
It is important to note that there is currently no cure for AIDS. Recent medical advantages have been made that have allowed AIDS to become a chronic and manageable condition. Currently researchers are working on the development of a vaccine, but until a vaccine is developed the primary goal of intervention will be focused on stopping HIV from replicating, to increase the number of CD4 cells, and to slow the progression of the disease. Antiretroviral Therapy (ART) is the current best medical management for individuals with HIV/AIDS. These drugs do not completely eradicate the virus and lifelong treatment is required until a method for permanent eradication is developed. In a study done by The Strategies for Management of Anti-retroviral Therapy (SMART) study group, it was concluded that episodic (meaning when the CD4 count dropped to 250 or below) therapy significantly increased the risk of opportunistic disease or death, as compared with continuous (ART when CD4 count is 350 or more). [10]
Non-pharmacological intervention include:
- Physical Therapy
- Nutritional counselling
- Exercise
- Mental health support
- Alternative and complimentary interventions
Physical Therapy Management
Physical Therapists play an important role in treating conditions that limit the patient’s movement and function. Goals will be set to improve the quality of life and keep the patient active in both his/her life and in the community. Patients with HIV develop many of the functional limitations that any other patient may have, such as sports-related injuries or arthritis. In addition to managing impairments, these patients may have problems with the disease process, infections, and/or side effects of the medication. A physical therapist will develop a plan of care to help the patient improve his/her ability to do daily activities, improve heart health, improve balance, reduce pain, and maintain healthy body weight. In addition, this plan of care, a proper home exercise program will be prescribed to achieve goals set by the patient or physical therapist. A qualitative study by deBoer et al.[11]suggests that collaborating physiotherapists on the interprofessional health care team would help in addressing the unique requirements of patients living with HIV.
In addition to improving the above mentioned positive benefits, the therapist must also address the following issues:
- Quality of life issues
- Work environment
- Community management skills (how to access transportation, socialisation opportunities, shopping, banking, ability to access and negotiate health care and insurance systems)
- Integumentary care
What Does the Literature Say
The current literature states aerobic exercise, progressive resistance exercise, or a combination may attribute to the following benefits:
- Performing constant or interval training for at least 20 minutes at least 3 times per week for at least 5 weeks appears to be safe and may lead to significant improvements in cardiopulmonary fitness (maximum oxygen consumption) body composition (leg muscle area, percent body fat) and psychological status. [12]
- Progressive resistance exercise appears to be safe and may be beneficial for medically-stable adults living with HIV. [12]
- PRE or a combination of PRE and aerobic exercise may lead to statistically significant increases in weight and arm and thigh girth. [13]
- Trends toward improvement in sub-maximum heart rate and exercise time were found. [13]
- HIV patients have abnormally low functional capacities, expressed as lowered capacity to utilize and perform physical work. [14]
- Low to moderate intensity exercise does not alter CD4 cell counts or viral load, nor does it increase the prevalence of opportunistic infections.[14]
- Higher intensity aerobic exercise training has been effective at improving Functional Aerobic Capacity. [14]
- All in all, fatigue remains the most frequent and debilitating complaint of HIV-infected people.[15] With this said, patients who partake in aerobic exercise, PRE, or a combination will begin to achieve the above mentioned benefits to combat fatigue.
In addition to progressive resistance exercise and aerobic exercise, physical therapist may also perform the following interventions to treat any impairment the patient may present with:
- Stretching
- Soft Tissue and Joint Mobilization
- Gait and Balance Training
- Functional Electrical Stimulation/Neuromuscular Electrical Stimulation
- Proprioceptive Neuromuscular Facilitation
- Desensitisation Techniques
The Benefits of Exercise
Exercise can provide the following benefits for patients suffering from HIV/AIDS:
- Pain relief
- Reduction of muscle atrophy
- Regularity of bowels
- Enhances immune function (by increasing T helper/ inducer CD4 cells and activating CD8 cells)
- Improves cardiovascular function
- Improves pulmonary function
- Improves endurance
- Helps prevent pneumonia and other respiratory infections
- Reduces anxiety and improves mood
Standard AIDS/HIV Precautions for Therapists and Other Health Care Workers: [5]
- Use protective barriers (gloves, glasses, gowns) when handling blood, body fluids, and infectious fluids.
- Wash hands and mucous membranes
- Prevent needle/scalpel sticks
- Use ventilation devices for resuscitation
- Don't treat a patient with HIV/AIDS if you have open wounds or skin lesions until lesions have healed.
- If pregnant take extra precautions
Outcome Measure for Quality of Life
Functional Assessment of HIV Infection (FAHI)
Differential Diagnosis
Many individuals with HIV/AIDS may remain asymptomatic for years, with a mean time of 10 years between exposure and development. Virtually, all the findings in the initial onset of AIDS may be found/mimic other diseases such as:
- Fever
- Headaches
- Night sweats
- Fatigue
- HTN
- Back pain
- Pulmonary complications ex. cough and SOA
- GI complaints (change in bowel habits and function)
- Cutaneous complaints (dry skin, new rashes, nail bed changes)
- Poor wound healing
- Thrush
- Easy Bruising
- Weight loss
- Herpes Simplex virus
- Cytomegalovirus
- Lymphoma
All of these signs/symptoms may be associated with other diseases, a combination of complaints is more suggestive of HIV infection than any one symptom alone. [6][7][16]
Related articles
Lessons from a seven-year experience of paediatric HIV in Pakistan: A single centre experience. – Physiospot – Physiotherapy and Physical Therapy in the SpotlightThe objective of this study was to describe demographic, clinical and immunologic features of children with human immunodeficiency virus. This descriptive study was conducted at the Shifa International Hospital, Islamabad, Pakistan, from 2005 to 2011, and comprised children with human immunodeficiency virus and acquired immune deficiency syndrome. Patients with detailed physical examination and appropriate investigations and those eligible for therapy were included. SPSS 21 was used for data analysis. Of the 43 patients, 27(62.8%) were boys and 16(37.2%) were girls. The overall median age was 5 years (interquartile range: 3-8.5 years). Moreover, 18(42%) children were aged equal to or below 5 years. Fathers of 5(12%) children and mothers of 6(14%) children had died. Siblings of 3(7%) patients, fathers of 20(47%) patients and mothers of 31(72%) patients had human immunodeficiency virus or acquired immune deficiency syndrome. The median duration of breastfeeding was 24 months (interquartile range: 15-24 months). Risk factors identified were foreign job by father in 12(28%) patients, birth by vaginal delivery in 20(47%), breastfeeding >6 months in 34(79%), fathers with human immunodeficiency virus or acquired immune deficiency syndrome in 20(47%), mothers with human immunodeficiency virus or acquired immune deficiency syndrome in 31(72%) and lack of maternal anti-retrovirals during pregnancy in all (100%). There were 27(63%) children being symptomatic and 29(67%) had advanced disease at diagnosis with World Health Organisation’s classification stage 3 or 4. The pretreatment median CD4 count was 294.5 cells/mm3 (IQR, 208.5-808) and a follow-up CD4 of 757 cells/mm3 (IQR, 352-874) which was significant (p <0.005). The intial median HIV viral load was 83 RNA copiesx105/mm3 (IQR, 1.8-8.25). Anti-retroviral therapy (ARV) was initiated in 65% (28/43) with good compliance. The mean duration of follow-up was 12 months. There was clinical and immunologic improvement in 65% (18/28) in first 12 months. There were opportunistic infections in 20 children (46%), serious side effects in 5 (18%), progression of disease or poor response in 7 (16%) and discontinuation or switch of therapy in 2 (7%). Four children had suspected HIV drug resistance but confirmed in 2 (6.7%) requiring second-line therapy. Five children (12%) died, two within one week of diagnosis. Most human immunodeficiency virus-infected children had risk factors, present with severe immune suppression and had improved CD-4 after anti-retroviral therapy.Functional Assessment of HIV Infection (FAHI) - PhysiopediaObjective The Functional Assessment of HIV Infection (FAHI) is a 47-item disease-specific instrument evaluating Health-Related Quality of Life (HRQL) in human immunodeficiency virus (HIV)-infected patients[1][2][3]. The FAHI is used for measuring Quality of life of People living with HIV.[3] Intended Population People living with HIV. Method of Use The FAHI evaluates physical well-being, functional and global well-being, emotional well-being/living with HIV, social well-being, and cognitive functioning. It yields a total score and individual subscale scores. Evidence The FAHI appears to be a reliable and valid measure for assessing quality of life in HIV-positive patients with concurrent drug and alcohol use disorders.[4]Non-Hodgkin's Lymphoma - PhysiopediaDefinition/Description Non-Hodgkin's lymphoma (NHL) is "a group of lymphomas affecting lymphoid tissue and occurring in persons of all ages."[1] "The lymphoid malignancies present as solid tumors arising from cells of the lymphatic system. The lymph nodes are usually involved first, and any extranodal lymphoid tissue, particularly the spleen, thymus, and GI tract, may also be involved. The bone marrow is commonly infiltrated by lymphoma cells, but this is rarely the primary site of a lymphoma. Lymphomas are classified according to the World Health Organization (WHO) which relies on the histochemical, genetic and cytologic features of the cells. Lymphomas are classified as either B-cell or T-cell lymphomas."[2] Other names for NHL include: Lymphocytic lymphoma, Histiocytic lymphoma, Lymphoblastic lymphoma. [3] Prevalence "NHL can affect any age range of individuals. It is more common in middle aged adults between the ages of 40 to 60."[1] "NHL comprises a large group of lymphoid malignancies (about 30 different specific types) and affects over 67,000 people per year, making this the 5th most common cancer in the United States."[2] In the United States in 2009, there were 65,980 new cases diagnosed and 19,500 deaths from non-Hodgkin lymphoma.[4] B-cell lymphomas: account for approximately 85% of non-Hodgkin lymphomas in the United States. [5] Diffuse large B-cell lymphoma: is one of the more common types on non-Hodgkin lymphoma in the U.S. and affects about 1 out of 3 cases (or 33%). Follicular lymphoma: affects about 1 out of 5 cases of non-Hodgkin lymphoma in the U.S. Small lymphocytic lymphoma: accounts for about 5% to 10% of all lymphomas. Mantle cell lymphoma: accounts for about 5% of lymphomas. Marginal zone B-cell lymphomas: account for about 5% to 10% of lymphomas. Primary mediastinal B-cell lymphoma: accounts for about 2% of all lymphomas. About 2 out of 3 people with this type are females in their 30s. Burkitt lymphoma: accounts for about 1% to 2% of all lymphomas. Close to 90% of patients with this type are males in their 30s. Lymphoplasmacytic lymphoma: accounts for 1% to 2% of all lymphomas. Hairy cell leukemia: is rare but accounts for about 1,000 people in the U.S. each year. T-cell lymphomas: account for less than 15% of non-Hodgkin lymphomas in the United States. [5] Precursor T-lymphoblastic lymphoma/leukemia: accounts for about 1% of all lymphomas. Peripheral T-cell lymphomas: are comprised of 7 different types of lymphoma and account for about 5% of all lymphomas. These include[5]: Cutaneous T-cell lymphomas (mycosis fungoides, Sezary syndrome)-- See Case Study Angioimmunoblastic T-cell lymphoma Extranodal natural killer/T-cell lymphoma, nasal type Enteropathy type T-cell lymphoma Subcutaneous panniculitis-like T-cell lymphoma Anaplastic large cell lymphoma Peripheral T-cell lymphoma Characteristics/Clinical Presentation "NHL presents in a similar manner as Hodgkin's disease, but NHL is usually more widespread and less predictable. The disease starts in the lymph nodes, although early involvement of the oropharyngeal lymphoid tissue or the bone marrow is common, as is abdominal mass or gastrointestinal involvement with complaints of vague back or abdominal discomfort."[1] "The most common manifestation is painless enlargement of isolated or generalized lymph nodes of the cervical, axillary, supraclavicular, inguinal, and femoral (pelvic) chains."[1] [2] "The development of these enlargements may occur slowly & progressively or rapidly depending on lymphoma type (indolent or aggressive)."[2] "Indolent disease may be minimally active & treatable for many years."[1] "Extranodal sites of involvement may include the nasopharynx, GI tract, bone, thyroid, testes and soft tissue. Abdominal lymphoma may cause abdominal pain & fullness, GI obstruction or bleeding, ascites, back pain & leg swelling. Lymph node enlargement in the chest can lead to compression of the trachea or bronchus, causing shortness of breath & coughing."[2] "Primary CNS lymphoma is a NHL restricted to the nervous system. Presenting symptoms may include: headache, confusion, seizures, extremity weakness/numbness, personality changes, difficulty speaking & lethargy. (Prior to the spread of HIV, this type of lymphoma was rare.)"[2] Clinical Signs and Symptoms of NHL Enlarged lymph nodes Fever Night Sweats Pallor Fatigue Weight Loss Bleeding Infection Red skin & generalized itching of unknown origin Pain in the chest, abdomen or bones for unknown reason[1][2][4] Associated Co-morbidities "Studies in the 1990s linked NHL to two widespread environmental contaminants: exposure to benzene & polychlorinated biphenyls (PCBs). Benzene can be found in cigarette smoke, gasoline, industrial pollution & 70% comes from automobile emissions. PCBs are found throughout the food chain (highest in meats, dairy & fish products)."[2] The development of NHL secondary to immunodeficienies may be due to a decrease in the host's surveillance mechanism against transformed cells and their inability to mount an adequate immune response (attack).[2] Risk Factors for Malignant Lymphomas Age (increased risk with increasing age)[1] Gender (males are more likely than females) Ultraviolet light exposure[2] Blood transfusions A diet high in meats, dairy, fish or fats Past treatment for Hodgkin lymphoma Environmental Contaminants Benzene Herbicides & Pesticides Polychlorinated biphenyls (PCBs) Radiation (including chemotherapy for another cancer) Viral Infection Epstein-Barr virus (EBV), mononucleosis virus HIV Human T-lymphotrophic virus type I (HTLV-1) Congenital Immunodeficiency Syndromes Hepatitis C Immunocompromise/immunodeficiency: Chronic disease or illness; autoimmune diseases Immunosuppresants Cancer treatment with alkylating or cytotoxic agents Inherited immune deficiencies AIDS Obesity (women) Methotrexate (used to treat rheumatoid arthritis, RA) Helicobacter pylori bacteria (gastric lymphoma) Medications/Treatment "Treatment varies for NHL depending on the type of lymphoma. In general, fast-growing tumors can be cured but require aggressive treatment; whereas, slow-growing tumors often cannot be cured, but the clinical course is chronic and the therapy is often reserved until symptoms develop. Localized disease may be treated with radiation, whereas disseminated disease requires radiation and chemotherapy."[2] Information about the drugs used in the treatment of NHL can be found at this link: Non-Hodgkin's Lymphoma Medication. [6] Common Chemotherapy Drug Treatments "The most common chemotherapy combination is CHOP (cyclophosphamide, doxorubicin, vincristine & prednisone). Another combination omits the doxorubicin (because of the effects on the heart) and is called CVP. Other agents include chlorambucil, fludarbine, & etoposide. Since many risk factors for NHL are associated with a reduced immune system, immune modulators, such as interferon and monoclonal antibodies, have been employed to combat NHL."[2] "Combining the monoclonal antibody rituximab (Rituxan)[7] with chemotherapy (CHOP) has produced high rates of response and is the treatment of choice for many NHLs. Clinical studies suggest that the immune modulator rituximab may alter the sensitivity of B-cell lymphoma to chemotherapy as well as induce apoptosis and cause the lysis of B cells."[2] "Bone marrow transplant (BMT) may be used for patients who replace or do not completely respond to treatment (which often occurs with aggressive lymphomas). Combined with intensive chemotherapy, BMT can be curative. In 2002, 4,300 BMTs were performed."[2] "For some lymphomas, chemotherapy becomes palliative because of an inability to overcome drug resistance within the lymphoma cells; attempts at overcoming specific drug resistance mechanisms have had limited success. Other strategies involve the use of antigen-presenting cells for taking up, processing, & presenting tumor protein in a vaccine strategy. This may provide a new tumor cells that persist following therapy. Radioimmunotherapy, radioactive labeling of a monoclonal antibody, is also under investigation to provide targeted therapy & provide tumor-free grafts for transplant."[2] "The optimal management of women with NHL who are pregnant requires special considerations because of the poor prognosis without treatment. Treatment during the first trimester should be avoided due to the risk of harm to the fetus, but the patient should receive chemotherapy during the second and third trimester despite the potential risk to the fetus."[2] [8] Diagnostic Tests/Lab Tests/Lab Values Physical Exam & History: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient's health habits and past illnesses and treatments will also be taken.[4] Complete Blood Count (CBC):[4] includes the: number of red blood cells, white blood cells & platelets, amount of hemoglobin in the red blood cells, proportion of blood that is made up of RBCs Blood Chemistry Studies: blood sample is checked to measure the amount of certain substances released into the blood by organs & tissues in the body. An abnormal count can be associated with a sign of disease in the organ or tissue.[4] Lymph Node Biopsy: is viewed by a pathologist to look for cancer cells.[4] Bone Marrow Aspiration & Biopsy: is the removal of bone marrow, blood & a small piece of bone from the hip or breastbone.[4] Liver Function Tests: the blood is checked for the enzyme lactate dehydrogenase (LDH). LDH levels help determine the prognosis and chance of recovery.[4] "Accurate diagnosis is important because of the other clinical conditions that can mimic malignant lymphomas (infection, tuberculosis, SLE, lung & bone cancer). Molecular genetic techniques that take advantage of the clonal nature of this malignancy are now being used to better characterize & diagnose the lymphomas. A biopsy is required to confirm the underlying cause of persistent enlargement of lymph nodes present."[2] "CT scans of the chest, abdomen and pelvis are helpful in staging, while MRI is used to image the brain and spinal cord. Bone marrow may be examined for staging and peripheral blood may be tested, but blood abnormalities are not present until the disease is in an advanced stage. If clinical symptoms warrant, a lumbar puncture for spinal fluid may be performed. Immunohistochemistry, flow cytometry or cytogenetic testing is often done to distinguish one type of NHL from another."[2] "The gallium scan using radiotracer, gallium-67, uptake is 85% to 90% accurate to predict residual disease after chemotherapy and is able to differentiate between active tumor tissue and fibrosis. PET imaging is becoming more widespread and can be performed to aid in the initial diagnosis and help ascertain if a lymph node is malignant or benign. PET is also used following chemotherapy (frequently along with CT) to determine if the lymphoma is reduced in size and the treatment is effective."[2] Causes "Most lymphomas start in a type of white blood cells called B lymphocytes, or B cells. For most patients, the cause of this cancer is unknown. According to the American Cancer Society, a person has a 1 in 50 chance of developing non-Hodgkin's lymphoma. High-risk groups includes those who have received an organ transplant or who have a suppressed immune system."[3] "Several possible etiologic mechanisms are hypothesized for NHL. Immunosuppression, possibly in combination with viruses or exposure to certain infectious agents, could be the primary cause."[1] The other causes may be related to the associated risk factors. Prognosis "Good prognostic features include age under 60 years, limited disease at diagnosis (stage I or II), lack of extranodal disease, and a normal lactate dehydrogenase (LDH) level. Individuals with NHL survive for long periods when involvement is only regional. The presence of diffuse disease reduces survival time. The indolent lymphomas are usually systemic & widespread and a cure cannot be achieved, whereas intermediate and fast-growing lymphomas are more likely to be treatable & even curable but require aggressive therapy."[2] "The prognosis for people with high-grade lymphomas depends on their response to treatment. More specifically, DLBCL can be cured in 40% to 50% of clients with therapy, follicular lymphoma has a 5-year survival of 60% to 70% (although it is eventually fatal), 20% of patients with mantle cell are alive at 5 years, and Burkitt's lymphoma has a 50% 5-year survival with intensive therapy. In general, the 5-year survival rate for NHL is 63% and the 10-year survival rate is 49%."[2] "Traditionally high-grade NHL associated with AIDS was synonymous with an extremely poor prognosis. But the advent of antiretroviral therapy for HIV the survival rates have approached those seen in individuals without HIV. Prognostic indicators for decreased survival rates in HIV-NHL include age greater than 35 years, history of injection drug use, CD4 cell count less than 100/100 ml, a history of AIDS before the diagnosis of lymphoma stage III or IV disease, and/or elevated LDH levels."[2] Systemic Involvement Lymphoid tissue is in many parts of the body, thus lymphomas can start in numerous places. The major sites of lymphoid tissue are[4] Medical Management Radiation therapy uses high energy rays to carefully and safely kill cancer cells while attempting to avoid the destruction of healthy cells. 'Radiation therapy is used to try and cure cancer, control the growth and spread of cancer and relieve symptoms, such as pain. The most common type is external beam radiation therapy, which is a series of daily outpatient treatments to accurately deliver radiation to the cancer cells. Treatment sessions usually last less than 30 minutes. Total nodal irradiation is radiation delivered to all lymph nodes in the body. Total body irradiation is radiation delivered to the entire body, usually prior to any transplants to kill all remaining cancer cells.'[9] "Chemotherapy[10] is the use of drugs to kill cancer cells and shrink tumors. Chemotherapy drugs are designed to attack rapidly dividing cells. Therefore, the drugs are not specific to cancer cells and will also be cytotoxic to normal, noncancerous cells. Patient's experience serious side effect, often secondary to the destruction of healthy, normal, noncancerous cells. Common side effects include: nausea, vomiting, diarrhea, hair loss, weight loss, mouth sores, depression and leukopenia. More serious side effects include: neutropenia, anemia, peripheral neuropathy, thrombocytopenia, kidney and liver damage, tumor lysis and/or allergic reactions."[10] Common chemotherapy drugs are developed from two different agents: Alkylating Agent: A cytotoxic (toxic to cells) agent that inhibits cell division by reacting with DNA[10]. Nucleosides: These inhibit DNA and RNA replication and thereby prevent cancer cells from growing[10]. There is research being done to develop a vaccination against lymphoma.[11] The vaccine itself is made by extracting cells from lymph nodes and identifying a cancer marker, called an "idiotype," that is unique to each patient. This idiotype is then fused with chemicals designed to stimulate the immune system. This vaccine have shown promising results[12] but are not able to cure anyone who currently has lymphoma or prevent anyone from developing lymphoma. The vaccination is a form of chemotherapy and has shown significant success in lengthening the time period before the cancer returns. Physical Therapy Management "Exercise, even if it is only minimal physical exertion, increases heart rate and muscle flexibility. It can also boost the body’s tolerance to conventional lymphoma cancer treatments, such as, chemotherapy and radiation. Taking part in a daily exercise program can also help the patient gain a sense of physical control over their condition, and provide a healthy outlet for stress and anxiety. Exercise programs that combine range of motion with other light activities like resistance training and aerobic exercise will provide positive health benefits. The Borg Scale of Rating of Perceived Exertion (RPE) is most often used during exercise because of the limiting qualities of cancer treatments. A Flexibility Program is often implemented to help relieve joint stiffness and pain while helping maintain good range of motion. The benefits of stretching include: Enhancement in performance of everyday activities Improvement in mobility and independence Improvement and maintenance in posture and muscle balance Injury prevention Promotion of physical and mental relaxation The physical therapy intervention that is most effective in providing an increased quality of life and improved endurance is Aerobic Exercise. Helping patient's maintain an active lifestyle increases their chance of survival. Instructions in a home exercise program (HEP) that consists of ankle range of motion, lower extremity strengthening and aerobic exercise can help them maintain normal gait mechanics and allow a quicker recovery after treatment. The following links support the use of aerobic exercise: Palliative and Supportive Treatment: Randomized Control Trial[13] Effects of Physical Therapy on Acute Lymphoblastic Leukemia.[14] Differential Diagnosis The differential diagnosis of Non-Hodgkin Lymphoma involves the ruling out of obvious and common conditions as well as other possible malignancies. The exact diagnosis hinges on the histological findings and the opinion of an experienced hematopathologist.[15] "In patients with cervical adenopathy (enlargement or disease of glands), infections, including bacterial or viral pharyngitis, infectious mononucleosis and histoplasmosis must be excluded. Other malignancies, such as nasopharyngeal and thyroid cancers, can present with localized cervical adenopathy and axillary adenopathy is a common metastatic manifestation of breast cancer. Mediastinal lymphomatous involvement must be distinguished from infections, sarcoidosis and other thoracic neoplasms."[15] The two main presentations of NHL are enlarged lymph nodes or skin rashes. Other diagnoses can include: Infection Tuberculosis Systemic lupus erythematosus (SLE) Lung/Bone Cancer Hodgkin's Disease (HD) Other Cancers Other Dermatitis (skin disorders) Resources Video & Information booklet on Non-Hodgkin Lymphoma What you need to know about Non-Hodgkin Lymphoma A Case Study: Cutaneous T-Cell Lymphoma -- a type of Non-Hodgkin Lymphoma A discussion about the presence of Diffuse Large B-cell Lymphoma that manifests in the bone marrow -- DLBCL is a type of Non-Hodgkin LymphomaHepatitis A, B, C - PhysiopediaDefinition/Description Hepatitis is defined as inflammation of the liver. This inflammation may be caused by various diseases, toxins, or viral infections.[1] Hepatitis A is a contagious liver infection caused by the hepatitis A virus. It causes inflammation that affects your liver's ability to function.[2] It is the most common of the two hepatitis viruses enterically transmitted in the US and one of the two that is vaccine-preventable.[3] Hepatitis B is another contagious liver infection that is caused by the Hepatitis B virus. The virus can cause an acute, short-term, infection that may last for several weeks or months. The virus and infection may also lead to chronic infection, leading to a long-term illness.[1] Hepatitis C is an infection caused by a virus that attacks the liver and leads to inflammation. Most people who have the infection often do not know that they have the disease, and are often asymptomatic. It is considered to be among the most serious of the hepatitis viruses.[4] About 80% of people who have the virus develop chronic hepatitis and many people also can develop cirrhosis or even liver cancer.[5] Prevalence About 3,600 cases of Hepatitis A are reported each year. However, since not all people are symptomatic, more people are infected than are diagnosed and reported.[6] Estimates for the prevalence of the Hepatitis B virus claim that more than one-third of the world's population has been infected with 5% of the population being chronic carriers.[7] Approximately 25% of all carriers will develop a serious liver disease, while there are over one million deaths due to the infection of the Hepatitis B virus.[7] According to the CDC, there were an estimated 43,000 new Hepatitis B infections in the United States in 2007, with the number of acute infections significantly declining. [1] For chronic infections, estimates range from 800,000-1.4 million people in the United States.[1] Every year around 3-4 million people are infected with the Hepatitis C virus. About 150 million people are chronically infected and at risk of developing liver cirrhosis and even liver cancer. More than 350,000 people die from hepatitis C-related liver disease every year.[8] Characteristics/Clinical Presentation Hepatitis A Hepatitis B Hepatitis C Symptoms usually do not appear until 2-6 weeks after you have been exposed to the virus. They are usually mild, but can last up to several months (2-6 months), especially in adults It is important to note that not everyone will develop signs and symptoms of the virus.[6] A vaccination is recommended for children age 12-23 months and for adults who are at high risk for the infection.[3] Acute infections may present with no symptoms, present with a gradual onset of symptoms in a few days-weeks, or present with symptoms very quickly.[9] Adults and children older than 5 are most likely to show symptoms of an acute Hepatitis B infection typically within 90 days of the exposure, but may show between 6 weeks and 6 months of the exposure to the virus.[1][9] Acute symptoms may last several weeks or up to 6 months.[1] Chronic Hepatitis B infection may result in ongoing symptoms or may be symptom free for as many as 30 years.[1] Early on, Hepatitis C usually is asymptomatic. When signs and symptoms begin to set in, they are generally mild and flu-like. About 75-85% of recently infected people develop chronic disease and 60-70% of chronically infected people develop chronic liver disease. Also 5-20% develop cirrhosis and 1-5% die from cirrhosis or liver cancer.[8] 1. Dark urine 2. Fatigue 3. Itching 4. Loss of appetite 5. Low-grade fever 6. Nausea and vomiting 7. Pale or clay-colored stools 8. Jaundice 9. Abdominal pain 10. Headache 11. Diarrhoea 12. Muscle Pain[2] 1. Fever 2. Fatigue 3. Loss of appetite 3. Nausea and vomiting 4. Abdominal Pain 5. Dark urine 6. Clay-colored bowel movements 7. Muscle[9] and joint pain 8. Jaundice 9. Symptoms of liver damage for chronic infections 1. Fatigue 2. Fever 3. Nausea or poor appetite 4. Muscle and joint pains 5. Tenderness of your liver[4] 6. Abdominal pain 7. Dark urine 8. Grey-coloured faeces 9. Jaundice[8] 10. Abdominal swelling 11. Itching[10] Associated Co-morbidities Some co-morbidities that may be associated with Hepatitis A, B, C include: Diabetes Obesity HIV ESRD Maladaptive lifestyle habits Poor quality of life[11] Liver disease Disorders of lipid metabolism Non-traumatic joint disorders GI disorders[12] Alcoholism Blood-clotting disorders Hypertension[13] Aetiology/Causes Hepatitis A Hepatitis B Hepatitis C Cause Hepatitis A virus Hepatitis B virus Hepatitis C virus Method of transmission Mostly found in stools and blood of infection person and is therefore spread primarily via person-to-person contact. Hepatitis A can spread when a person unknowingly ingests the virus from objects, food, or drinks contaminated by small, undetected amounts of stool from an infected person. (CDC) Hepatitis A can also spread from close personal contact with an infected person such as through sex or caring for someone who is ill. Spread through contact with body fluids such as semen, vaginal fluids, saliva, and blood.[1][9] Spread when come into contact with contaminated blood. Contracted when exposed to: 1. Food or drink that has been contaminated by stools containing the Hepatitis A virus 2. Contact with stool or blood of a person infected 3. A person with the disease does not wash his/her hands properly after using the restroom and touches other objects or foods 4. Participating in sexual practices involving oral-anal contact with an infected individual[6] 1. Childbirth- passed from mother to child 2. Sexual contact from unprotected intercourse 3. Shared needles- injection drug use or those given contaminated with syringes an needle-stick injuries in healthcare settings 4. Sharing personal items such as razors or toothbrushes with an indivdual infected 5. Direct contact with blood or an open sore of an individual infected[1] 6. Any blood or bodily fluid touches skin, eyes, or mouth[9] 1. Blood transfusions and organ transplants before 1992. 2. Shared needles- injection drug use or those given with contaminated syringes and needle-stick injuries in health-care settings 3. Childbirth- passed from mother to child 4. Sexual contact from unprotected intercourse 5. Long-term kidney dialysis 6. Regular contact with blood work 7. Sharing personal items such as razors or toothbrushes with an individual infected[10] Risk Factors 1. Travelling 2. Native people of America 3. Restaurant workers and food handlers 4. Children living in communities that have high rates of the disease 5. Children and workers in day care facilities 6. Individuals engaging in anal/oral sex with STDs or HIV 7. People with chronic liver disease 8. If you eat raw shellfish frequently 9. Laboratory workers who handle live Hepatitis[3] 1. Unprotected sexual intercourse with an infected partner 2. Blood transfusions (uncommon in the United States) 3. Contact with blood at work 4. Long-term kidney dialysis 5. Receiving a tattoo or acupuncture with an unclean needle 6. Sharing needles during drug use 7. Sharing personal items with an infected individual 8. Were born to a Hepatitis B infected mother[1][9] 9. Travelling to countries with high rates of the virus 10. Men who have sexual contact with other men 11. Living with a person infected with chronic Hepatitis B[1] Systemic Involvement Variable systemic involvement can occur with Hepatitis due to the nature of the virus causing a widespread infection in the body. Most predominantly the infection involves the liver and lymphatic system. Other systemic areas of involvement include progression into renal, endocrine, dermatological, cardiovascular, rheumatologic, and central nervous system diseases.[14] Diagnostic Tests/Lab Tests/Lab Values A primary care physician will conduct a physical exam when looking for Hepatitis A Virus. During the physical exam, they may find that you have an enlarged and tender liver. Also, they will have you partake in blood tests. The blood tests will look at IgM and IgG antibody levels as well as liver enzymes. In both cases, the antibody and enzyme levels will be raised.[6] Blood tests are done to check for the Hepatitis B virus. The blood tests available may include:[1] Hepatitis B Surface Antigen HBsAG Positive test means the person has an acute or chronic infection and can transmit the virus to others. Hepatitis B Surface Antibody anti-HBs Positive test means a person is immune from getting the virus. Total Hepatitis B Core Antibody anti-HBc Positive test means a person is currently or previously has been infected. IgM Antibody to Hepatitis B Core Antigen IgM anti-HBc Positive test means a person has been infected within the past 6 months. Hepatitis B "e" Antigen HBeAg Positive test means a person has high levels of the virus in the blood and can spread the virus to others easily. Hepatitis B e Antibody HBeAb or anti-HBe Positive test means a person has a chronic infection but have low levels of the virus in their blood. Hepatitis B Viral DNA Positive test means the virus is multiplying and is highly contagious or the person has a chronic infection with an increased risk for liver damage. Blood tests are also done to check for the Hepatitis C Virus. They specifically look at EIA assay to detect the hepatitis C antibody and the hepatitis C RNA assay to measure virus levels. Genetic testing can be done to check for the hepatitis C genotype. Six different genotypes exist. Most people have genotype 1 infection, which is the hardest to treat. Genotypes 2 and 3 are also common, but typically respond better to treatment. Tests can also be done to monitor the amount of liver damage: albumin levels, liver function tests, and prothrombin time. A liver biopsy can also be done to assess liver damage.[10] Management Medical Management Hepatitis A There is no specific treatment for Hepatitis A. Rest is recommended when the symptoms are most severe. Individuals with acute hepatitis should avoid alcohol and any substances that are toxic to the liver, such as Tylenol. Fatty foods that can cause vomiting should also be avoided during the acute phase.[6] It is important to maintain comfort and an adequate nutritional balance as recovery can take several weeks up to a month. It is also important to constantly replace fluids that you may be losing.[15] It is most important to prevent contracting the disease. Sexual activities should be avoided with an individual who has Hepatitis A, as a condom does not offer adequate protection. Also, wash your hands thoroughly after using the toilet, whether a person is infected or not. Refrain from preparing food for others while one is infected, as this way the disease is passed on.[2] Also avoid unclean food or water, especially if travelling.[6] Hepatitis B There is no available treatment for acute Hepatitis B infections. Patients with acute infection are recommended to rest and get an adequate nutritionally intake of food and fluids. Individuals with chronic Hepatitis B medical management will involve medical monitoring, abstinence from alcohol, and antiviral therapy in order to suppress the infection and end the active liver disease. These individuals should avoid consumption of alcohol completely because it makes the liver disease worse. Antiviral therapy is appropriate for patients with a chronic Hepatitis B infection who have tested positive for hepatitis B surface antigen for at least six months, have abnormal blood levels of liver enzymes, actively dividing virus in the blood, and a liver biopsy showing moderate disease activity.[16] Antiviral therapy helps in preventing further liver damage.[17] Approved drugs for Hepatitis B include:[18][17][19] Method Adverse Side Effects Interferon Alpha Injection Multiple times per week for 6 months-1 year flu-like symptoms, depression, headaches Pegylated Interferon used with high levels of the virus to stimulate the immune system Injection Once weekly for 6 months-1 year flu-like symptoms, depression, various persistent unpleasant side effects Nucleoside Analogs prevent the virus from spreading by preventing the genetic code from being copied Tenofovir Oral Once-daily for at least 1 year diarrhoea, nausea, skin rash, feeling of weakness, dizziness Entecavir nausea, insomnia, dizziness Lamivudine Adefovir Dipivoxil Telbivudine few side effects but not recommended as first line of treatment due to high rate of viral resistance Hepatitis C Hepatitis C does not always require treatment. There are 6 genotypes of Hepatitis C and they all respond differently to a treatment. A good screening is required before starting the treatment to determine the most appropriate approach. Combination of antiviral therapy with interferon and ribavirin has been the most common form of treatment for Hepatitis C. Interferon is not widely available globally and is not well tolerated depending on the genotype the patient presents with. Therefore, not all patients finish their interferon treatment. Two new drugs have been developed that may be better tolerated and they are telaprevir and boceprevir. However, more testing needs to be done to ensure that these new drugs lead to greater access and treatment globally.[8] Since the Hepatitis C virus infects the blood and can lead to cirrhosis of the liver or liver cancer, the goal of medication is to prevent this from happening. Many patients with hepatitis C benefit from treatment with medications similar to Hepatitis B. The most common medication include antiviral medications including pegylated interferon alfa and ribavirin. Typically pegylated interferon alfa is received weekly through injections. Ribavirin is a capsule taken twice daily. Treatments are given from 24-48 weeks. Two newer drugs that may be available for use for patients with genotype 1 are Telaprevir and Boceprevir. These medications do have several side effects, and therefore, patients need to be watched closely. Some of the side effects of the medications can include depression and flu-like symptoms. If the liver has been severely damaged, a liver transplant may be an option. It is important to realize that a liver transplant is not the cure and the use of antiviral medications continues after the liver transplant takes place.[4] [10] It is also recommended that people be careful not to take vitamins, nutritional supplements, or new over-the-counter medications without first discussing it with their primary care physician. It is important to avoid any substances that are toxic to the liver such as alcohol, as it can speed up the progression of the disease. Prevention With all three of the diseases preventing contraction of the virus, and therefore the infection is key. Prevention can help avoid passing on the disease or contracting the illness. The risk of infection can be reduced by: Receiving Hepatitis A and B vaccines Avoiding unnecessary and unsafe injections Avoiding unsafe blood products Avoiding unsafe sharps and waste collection and disposal Avoiding the use of illicit drugs and sharing injection equipment Avoiding unprotected sex with infected individuals Avoiding the sharing of sharp personal items that may be contaminated with infected blood Avoiding tattoos, piercings, and acupuncture performed with contaminated equipment[8][1] Vaccines If you have been exposed to the Hepatitis A infection and have not had it before or have not received the vaccine, ask your doctor or nurse about receiving either immune globulin or the Hepatitis A vaccine. Vaccines that protect against the virus are available and begin to protect you for weeks after receiving the initial dose. The 6-12 month booster is required for long-term protection.[6] It is especially important that children age 12-23 months or adults at high risk for contracting the virus get a vaccine. Also it is important for anyone one year of age and older traveling to or working in countries with high or intermediate prevalence of Hepatitis A (central or south America, Mexico, Asia), children and adolescents 2-18 who live in states or communities where routine vaccination has been implanted because of high disease prevalence, men who have sex with men, people who use street drugs, people with chronic liver disease, people who are treated with clotting factors, and people who work in HAV laboratories to get vaccinated for safety reasons.[20][10] Hepatitis B can be prevented in 95% of recipients with the proper vaccine.[7] Individuals who believe they may have contracted the Hepatitis B virus can receive the Hepatitis B vaccine, the Hepatitis B immune globulin, within 24 hours to potentially prevent infection.[1] A surface antigen of the Hepatitis B virus is what makes up the vaccine. These vaccines are produced by two methods: plasma-derived or recombinant DNA.[7] All individuals suffering from chronic liver diseases, such as Hepatitis B and C, should receive Hepatitis A immunization as well as the Hepatitis B immunization.[16] Physical Therapy Management A multifaceted approach is needed in the treatment of Hepatitis A, B, and C. No specific physical therapy intervention is appropriate for the specific infection of Hepatitis, but Hepatitis may likely be a comorbidity of a patient seen in physical therapy. With any other medical condition, it is important to educate patients on their disease and risk factors to promote awareness and improvement in their healthy lifestyle. In physical therapy, an emphasis on proper musculoskeletal health will be an important foundation for the patient's overall health. Stretching to improve flexibility could help alleviate symptoms of muscle pain. It is also important for the patient to remain physically active in order to maintain the healthiest lifestyle possible and prevent the patient from developing secondary co-morbidities due to inactivity. General strengthening and aerobic activity might be appropriate for a deconditioned patient. Individualizing a physical therapy program focusing on the impairments of the patient is of utmost importance for any patient. During physical activity, it is important to monitor the patient for signs and symptoms of fatigue. For Hepatitis A bed rest is the recommended form of treatment and being aware of the acuteness of the Hepatitis infection is important when screening for physical therapy. Supportive therapy and patient education are used to ensure the patient is comfortable and has an adequate nutritional balance for all three infections. It is also important to remind the patient to refrain from the use of alcohol or intake of fatty substances.[15] Differential Diagnosis Differential diagnosis for acute Hepatitis includes:[21] Epstein-Barr Virus: leads to infectious mononucleosis with presenting symptoms of fever, sore throat, swollen lymph glands, swollen liver or spleen, jaundice, right upper quadrant pain[22][23] Cytomegalovirus: usually affecting infants where the symptoms of the infection vary[24] Alcoholic Hepatitis: jaundice, scleral icterus, muscle wasting, ascites, oedema, spider angiomata, asterixis, Drug-Induced Liver Injury Mushroom Ingestion: stomachaches, drowsiness, confusion, gastrointestinal issues, heart, liver or kidney damage[25] "Shock Liver:" low cardiac output leading to hepatic ischemia presenting with low blood pressure to cause weakness and lightheadedness and liver damage[26] Differential diagnosis for chronic Hepatitis includes:[21] Non-alcoholic steatohepatitis: diagnosed by excluding other causes and the presence of a fatty liver because there are few symptoms of the disease that could possibly include fatigue, weight loss, weakness, cirrhosis in late stages[27] Chronic Alcoholic Hepatitis: pain and swelling in abdomen, decreased appetite and weight loss, nausea and vomiting, fatigue, dry mouth, increased thirst, bleeding of the esophagus, jaundice, spider-like veins, dry or pale skin, redness of feet/hands, itching, cognitive issues, fainting, numbness in legs and feet[28] Primary Biliary Cirrhosis: inflamed and damaged bile ducts presenting with fatigue, pruritus, dry eyes/mouth, jaundice[29] Primary Sclerosing Cholangitis: swelling and scarring of bile ducts presenting with fatigue, itching, jaundice, enlarged liver or spleen, weight loss, repeat cholangitis[30] Hereditary Hemochromatosis: genetically inherited iron overload disease presenting with joint pain, fatigue, abdominal pain, loss of sex drive, cardiovascular issues[31] Wilson's Disease: genetically inherited disease of copper overload presenting with swelling of the liver or spleen, jaundice, fluid buildup in the legs/abdomen, easily bruised, fatigue, physical coordination, tremors, muscle stiffness, behavioral changes, anemia, low platelet count, low WBC count, slower clotting time[32] Alpha-1-antitrypsin deficiency: genetically inherited disease that presents as lung disease but can be associated with liver disease and cirrhosis of the liver[33] Celiac Disease: condition that damages the lining of the small intestine to prevent absorption of parts of food that presents with abdominal pain, constipation, decreased appetite, lactose intolerance, diarrhoea, nausea and vomiting, unexplained weight loss, stools that float or are foul-smelling, bruising easily, depression, fatigue, delay of growth, hair loss, itchy skin, missed menstrual periods, mouth ulcers, muscle cramps, joint pain, nosebleeds, seizures, tingling/numbness in hands/feet[34] Primary liver cancer Metastatic cancer Herpes Simplex Virus: visceral involvement in infants and pregnant women specifically the oesophagus, lungs, and liver with HSV viremia[23] Varicella-Zoster Virus: generalized rash is typical but can also present with encephalitis, pneumonitis, myocarditis, and hepatitis[23] Human Parvovirus: can present with haematological disorders that may present similar to hepatitis[23] Alternate diagnosis for Hepatitis A Some alternate diagnoses for Hepatitis A that could be made based on the presenting signs and symptoms could be: Budd-Chiari Syndrome: uncommon condition induced by thrombotic or non-thrombotic obstruction to hepatic venous outflow. Hepatomegaly, ascites, and abdominal pain are characteristics of the disorder[35] Cytomegalovirus: resulting in fever of unknown origin, pneumonia, hepatitis, encephalitis, myelitis, colitis, uveitis, retinitis, and neuropathy[36] Other Hepatitis Virus[37] Differential diagnosis for Hepatitis B include:[38] Alcoholic liver disease Non-alcoholic fatty liver disease Autoimmune hepatitis Metabolic and genetic disorders Drug-induced liver disease Granulomatous disorders Differential diagnosis for Hepatitis C are: Alcohol Liver Disease: Complications such as oesophageal or gastric variceal bleeding, ascites, coagulopathy, hepatic encephalopathy, and liver cancer are associated with the disease.[39] Hepatic Steatosis: Non-alcoholic hepatic steatosis, or non-alcoholic fatty liver disease, is the most common cause of chronic liver disease.[40] Hemochromatosis: An autosomal-recessive disorder of inappropriately increased dietary iron absorption and increased iron release from erythrophagocytosis; Presenting features include fatigue, arthralgias, and diabetes mellitus[41] Other Chronic Liver Dieases[42] Autoimmune Hepatitis: Autoimmune hepatitis is a chronic disease of unknown cause, characterized by continuing hepatocellular inflammation and necrosis and tending to progress to cirrhosis.[43] Cholangitis: an infection of the biliary tract with the potential to cause significant morbidity and mortality.[44] Viral Hepatitis[45] Case Reports/ Case Studies Hepatitis C Case Study Resources Chronic Liver Disease Foundation Hepatitis Central Hepatitis A Vaccine Information Sheet Hepatitis B Foundation Resources and Links Hepatitis B Advocate Hepatitis C Virus AdvocateCommunicable Diseases - PhysiopediaIntroduction According to the World Health Organisation “over 13 million people die each year from Infectious and Parasitic Diseases: One in two deaths in some developing countries. Poor people, women, children, and the elderly are the most vulnerable. Infectious diseases continue to be the world’s leading killer of young adults and children” [1]. Socioeconomic, environmental and behavioural factors, as well as international travel and migration, foster and increase the spread of Communicable Diseases. Vaccine-preventable, foodborne, zoonotic, health care-related and communicable diseases pose significant threats to human health and may sometimes threaten international health security [2]. According to Lindahl and Grace (2015) communicable diseases have had civilisation-altering consequences throughout history. An estimated 50–100 million humans worldwide succumbed to infection during the Spanish Flu Pandemic in 1918–1920. While rinderpest was in part responsible for death by starvation of almost two-thirds of the East African Massai population after it caused massive death to livestock. [3] As a result of better living conditions, increased access to health care including better vaccines, advent of antibiotics and improved surveillance and monitoring in relation to public health, the proportion of infectious diseases was trending downwards during the early Twentieth Century, however, an increase in the emergence and re-emergence of infectious diseases became evident in many parts of the world towards the later part of the Twentieth Century. [3] [4] Weiss & McMichael (2015) highlight that over 30 new, emerging diseases have been identified, including Legionnaires' Disease, Human Immunodeficiency Virus (HIV) / Acquired Immune Deficiency Syndrome (AIDS), Hepatitis C, Bovine Spongiform Encephalopathy (BSE) / Variant Creutzfeldt-Jakob Disease (vCJD), several Viral Hemorrhagic Fevers and, most recently, Severe Acute Respiratory Syndrome (SARS), Avian Influenza, Ebola and Zika Virus and in part relate the emergence of these diseases, and resurgence of old ones like Tuberculosis and Cholera to various changes in human ecology including rural-to-urban migration resulting in high-density peri-urban slums; increasing long-distance mobility and trade; the social disruption of war and conflict; changes in personal behavior; and, increasingly, human-induced global changes, including widespread forest clearance and climate change. [4] What are Communicable Diseases Communicable diseases are those that are spread from one person to another through a variety of methods. Socioeconomic, environmental and behavioural factors, as well as international travel and migration, foster and increase the spread of Communicable Diseases. Vaccine-preventable, foodborne, zoonotic, health care-related and communicable diseases pose significant threats to human health and may sometimes threaten international health security .How these diseases spread depends on the specific pathogen or infectious agent and means of transmission: [5] Pathogens Bacteria These one-cell organisms are responsible for illnesses such as strep throat, urinary tract infections and tuberculosis. Bacteria constitute approximately 38% of human pathogens, and 30% of the emerging pathogens in humans. [3] [6] Viruses Even smaller than bacteria, viruses cause a multitude of diseases. According to Lindahl & Grace (2015) it is estimated that 44% of the diseases considered emerging in humans are viral. Emerging Infectious Diseases that that have received most publicity in the past 30 - 40 years have been viruses. Notable examples have been HIV, SARS, and Ebola. [3] [6] Fungi Many skin diseases, such as ringworm and athlete's foot, are caused by fungi. Other types of fungi can infect your lungs or nervous system. [6] [3] Parasites According to the CDC, a parasite is an organism that lives on or in a host and gets its food from or at the expense of its host. Malaria is caused by a tiny parasite that is transmitted by a mosquito bite. Other parasites may be transmitted to humans from animal feces. [6] [3] [7] Prions A prion is an infectious agent composed entirely of protein material, called PrP (short for prion protein), that can fold in multiple, structurally distinct ways, at least one of which is transmissible to other prion proteins, leading to disease that is similar to viral infection. Bovine Spongiform Encephalopathy (BSE), also known as Mad Cow Disease, is a progressive neurological disorder of cattle that results from infection by an unusual transmissible agent called a prion. [3] Transmission Defining the means of transmission of a pathogen is important in understanding its biology and in addressing the disease it causes. Infectious organisms may be transmitted either by direct or indirect contact. Direct contact occurs when an individual comes into contact with the reservoir. Indirect contact occurs when the organism is able to withstand the harsh environment outside the host for long periods of time and still remains infective when specific opportunity arises. Direct Contact Person to Person: Physical Contact with an infected person, such as through Touch (e.g. Staphylococcus), Sexual Intercourse (e.g. Gonorrhea, HIV), Fecal/Oral Transmission (Hepatitis A), or Droplets (Influenza, Tuberculosis) Animal to Person: Bites from infected insects or animals capable of transmitting disease (e.g. Mosquito: Malaria, Zika Virus and Yellow Fever; Flea: Plague; Tick: Lyme Disease); and handling of animal waste (e.g. Toxoplasmosis) Mother to Unborn Child: Infectious Disease may be transmitted to the unborn child through the placenta or during passage through the vaginal canal during the birth process e.g. HIV, Hepatitis, Herpes, and Cytomegalovirus. Indirect Contact Contact with a contaminated surface or object (Norovirus), Food (Salmonella, E. Coli), Blood (HIV, Hepatitis B), or Water (Cholera); Travel through the air (e.g. Tuberculosis or Measles) Defense Mechanisms Host defenses that protect against infection include: Natural Barriers (e.g. Skin, Mucous Membranes) [8] Skin usually prevents invading microorganisms unless it is physically disrupted or broken (e.g. by Injury, IV Catheter, or Surgical Incision). Exceptions include the following: Mucous Membranes contain mucous membranes which produce secretions that have antimicrobial properties (e.g. cervical mucus, prostatic fluid, and tears containing lysozyme). Local secretions also contain immunoglobulins, principally IgG and secretory IgA, which prevent microorganisms from attaching to host cells. Respiratory Tract has upper airway filters which transport invading organisms away from the lung by the mucociliary epithelium. Coughing also helps remove organisms. If the organisms reach the alveoli, alveolar macrophages and tissue histiocytes engulf them. However, these defenses can be overcome by large numbers of organisms or by compromised effectiveness resulting from air pollutants (eg, cigarette smoke) or interference with protective mechanisms (eg, endotracheal intubation, tracheostomy). GI Tract barriers include the acid pH of the stomach and the antibacterial activity of pancreatic enzymes, bile, and intestinal secretions. Peristalsis also remove microorganisms, which if delayed can result in prolonged infection. Compromised GI defense mechanisms may predispose patients to particular infections (eg, achlorhydria predisposes to salmonellosis). Normal bowel flora can inhibit pathogens; alteration of this flora with antibiotics can allow overgrowth of inherently pathogenic microorganisms (eg, Salmonella Typhimurium) or superinfection with ordinarily commensal organisms (eg, Candida albicans). Nonspecific Immune Responses (e.g. Phagocytic Cells [Neutrophils, Macrophages] and their products) [8] Cytokines, produced principally by macrophages and activated lymphocytes, mediate an acute-phase response that develops regardless of the inciting microorganism. The response involves fever and increased production of neutrophils by the bone marrow. Inflammatory response directs immune system components to injury or infection sites and is manifested by increased blood supply and vascular permeability, which allows chemotactic peptides, neutrophils, and mononuclear cells to leave the intravascular compartment. Phagocytes, which are drawn to microbes via chemotacis, limit microbial spread through engulfment of microorganisms. Oxidative products such as hydrogen peroxide are generated by the phagocytes and kill ingested microbes. Specific Immune Responses (e.g. Antibodies, Lymphocytes) [8] The host can produce a variety of antibodies that bind to specific microbial antigenic targets. Antibodies can help eradicate the infecting organism by attracting the host’s WBCs and activating the complement system, which destroys destroys cell walls of infecting organisms. Antibodies can also promote the deposition of substances known as opsonins on the surface of microorganisms, which helps promote phagocytosis. Antimicrobial Resistance Antimicrobial resistance (AMR) threatens the effective prevention and treatment of an ever-increasing range of infections caused by bacteria, parasites, viruses and fungi and according to WHO is an increasingly serious threat to global public health that requires action across all government sectors and society. Without effective antibiotics, the success of major surgery and cancer chemotherapy would be compromised. [9] Antimicrobial resistance happens when microorganisms (such as bacteria, fungi, viruses, and parasites) change when they are exposed to antimicrobial drugs (such as antibiotics, antifungals, antivirals, antimalarials, and anthelmintics). Microorganisms that develop antimicrobial resistance are sometimes referred to as “superbugs”. As a result, the medicines become ineffective and infections persist in the body, increasing the risk of spread to others. [9] While antimicrobial resistance occurs naturally over time, usually as a result of genetic changes, misuse and overuse of antimicrobials bu both humans and animals, is accelerating this process. Examples of misuse include when they are taken by people with viral infections like colds and flu, and when they are given as growth promoters in animals and fish. [9] Refresh your knowledge of some common communicable diseases: Pneumonia HIV/AIDS Tuberculosis Malaria Review your knowledge of Antibiotic Resistant Infectious Diseases which are frequent within the Hospital Setting Methicillin-Resistant Staphylococcus Aureus (MRSA) Clostridium Difficile Infection (CDif) You can also check out our Infectious Disease Category which provides information on many other common and not so common Infectious Conditions: Infectious Diseases Risk Factors According to Boundless (2016) the spread and severity of infectious disease is influenced by many predisposing factors. Some of these are more general and apply to many infectious agents, while others are disease specific. Some predisposing factors of contracting infectious diseases can be anatomical, genetic, general and disease specific. Climate and weather, and other environmental factors that are affected by them, can also predispose people to infectious agents. Other factors such as overall health, age and diet are also important considerations in the prevention of spreading infectious diseases [10]. Modifiable Risk Factors Refer to characteristics that individuals or societies can change to reduce risk of infectious disease and improve health outcomes. which include Hygiene including water and sanitation, Vaccinations, Malnutrition, Food Preparation Methods and Overcrowding. Overcrowding High Population Density provides greater opportunity for contact between infectious diseases and susceptible people which leads to higher transmission rates. Large Concentration of Population once an epidemic starts, it spreads faster which leads to higher transmission rates. According to WHO from a purely epidemiological perspective, providing sufficient residential space and avoid of overcrowding provide high-impact public health interventions to reduce rate of transmission of communicable disease Types of Diseases: Airborne Droplet Diseases e.g. Measles, Meningitis, Acute Respiratory Infections, and Tuberculosis. Faecal-Oral Diseases e.g. Diarrhoea Diseases including Shigella and Cholera Malnutrition Malnutrition leads to lower natural immunity, which often results in increased risk of infectious disease and increased progression of disease. Nutritional Crises can Precipitate Epidemics as lower immunity often means lower vaccine efficacy, and therefore a higher susceptibility for transmission Globally, the severe malnutrition common in parts of the developing world causes a large increase in the risk of developing active tuberculosis and other opportunistic infections, due to its damaging effects on the immune system. Along with overcrowding, poor nutrition may contribute to the strong link observed between tuberculosis and poverty. [10] Lindahl and Grace (2015) consider the factors that impact on the number of individuals susceptible to infection, the factors leading to increased exposure and the factors related increased risk of infectivity. A new population can become at risk for an infection if a new pathogen is transferred to a previously uninfected area. This both can occur as a result of migration or travel over a distance where a pathogen is brought by an infected individual, in a vector, or in contaminated products, and it can be a slow progression into neighbouring areas, by animal, human, or vector movements. Cultural exchange may also cause a population to adopt new habits and acquire new risks. The framework showing factors contributing to increased susceptible populations is shown in Fig. 1. Figure.1 Factors Leading to Increases in the Number of Susceptible Individuals [3] A major factor in the risk of exposure to a pathogen already in place is the pattern of interaction between individuals, which depends on the population density and behaviour. Increasing urbanization, as well as intensified animal keeping, increases exposure. A framework showing factors contributing to increased exposure is shown in Fig. 2. Figure.2 Factors Leading to Increased Exposure to Infectious Diseases [3] How infectious an individual is following an infection, and for how long, is dependent on factors in the infected individual, on the pathogen, and the possibility of veterinary and medical care to cure the infection. A framework showing factors contributing to increased infectivity is shown in Fig. 3. Figure.3 Factors Contributing to Increased Infectivity [3] Signs & Symptoms Depending on the etiology (eg. virus, bacteria), the systems involved (e.g. respiratory, cardiovascular, central nervous system) and stage of disease (e.g. acute, chronic) the clinical manifestations of Communicable Diseases will vary widely and may be local to the site of infection (eg, cellulitis, abscess) or systemic (most often fever). Manifestations may also develop in multiple organ systems and severe, generalised infections may have life-threatening manifestations (eg, sepsis, septic shock). [11] [5] Cardiovascular Tachycardia Bradycardia Hypotension Tachypnea Dyspnea Cough Hoarseness Sore Throat Nasal Drainage Sputum Production Oxygen Desaturation Decreased Activity/Exercise Tolerance Central Nervous System Altered Consciousness Confusion Delirium Stupor Coma Seizure Headache Photophobia Memory Loss Stiff Neck Myalgia Endocrinology Increased Thyroid-stimulating Hormone Increased Vasopressin Increased Insulin Increased Glucagon Hyperglycemia Hypoglycemia Gastrointestinal Nausea Vomiting Diarrhea Geniturinary Heamaturia Dysuria Oliguria Proteinuria Urgency Frequency Haematology Increased Immature Neutrophils Increased Mature Neutrophils Release Granulocytes Increased Leukocytes Thrombocytopenia Integumentary Purulent Drainage Skin Rash Red Streaks Bleeding from Gums Bleeding into Joints Erythema Joint Effusions Systemic Fever Chills Malaise Enlarged Lymph Nodes Changes in Mental Status Fatigue Lethargy Altered Appetite Implications for Physiotherapy As healthcare workers it is important that we recognise the symptoms of the most important infectious diseases and direct those affected to appropriate treatment as quickly as possible. It is also important to be aware of the role physiotherapy has in treating and advising patients presenting with these diseases. For example: the benefits of exercise for patients with HIV/AIDS[12][13], treatment of motor-function disability following cerebral malaria[14], reduced risk of ventilator-associated pneumonia[15][16]. use of mechanical airway clearance in patients with pulmonary tuberculosis[17] rehabilitation of disabilities resulting from diseases the Zika Virus[18] and Ebola Virus[19][20] The statistics related to HealthCare Associated Infections make it clear Hand Hygiene in the healthcare environment is extremely important. As physiotherapists we need to learn how to use the alcohol hand rubs effectively and utilise these frequently. The WHO Guidelines identify 5 moments for Hand Hygiene: Before Touching the Patient Why? Protect the patient from acquiring germs that might be on your hands. Clean your hands prior to personal care activities like bathing, dressing, brushing and oral care, as well as non-invasive observations (taking vital signs) and treatments. Before Clean/Aseptic Procedure Why? Protect the patient from harmful germs, including their own, that could enter the body during procedures like needle insertions, medication administration and connecting to invasive medical devices like EEGs. After Body Fluid Exposure Risk Why? Protect yourself and the patient’s surroundings from harmful patient germs generated via contact with fluids like blood, saliva, mucous, semen, tears or urine. After Touching a Patient Why? Protect yourself and the immediate environment from harmful patient germs. After you touch a patient, you could have microorganisms on your hands that would get passed on to other patients. After Touching Patient Surroundings Why? Protect yourself and the immediate surroundings from harmful patient germs. [21] [22] Resources Guidelines & Policy World Confederation for Physical Therapy. Policy Statement Infection Control & Prevention. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4353090/. [Accessed: 11 Jan 2017] Open Access Journals Antimicrobial Resistance & Infection Control. Published by one of the largest reputable open-access journal providers, BioMed Central, ARIC investigates the factors behind the development of multidrug resistant pathogens. International Journal of Infectious Diseases. This official journal of the International Society of Infectious Diseases became completely open access at the start of 2014 and publishes important research each month. Emerging Infectious Diseases. The fourth most influential journal for infectious disease research, this monthly publication from the Centers for Disease Control has been disseminating key HIV/AIDS research for decades, as well as information on other infectious diseases. Consensus Papers & Relevant Articles Mills A, Shillcutt S. Copenhagen consensus challenge paper on communicable diseases. Copenhagen Consensus Challenge Paper. 2004. Barber NC, Stark LA. Online resources for understanding outbreaks and infectious diseases. CBE-Life Sciences Education. 2015 Mar 2;14(1):fe1 Hand Hygiene Resources Centers for Disease Control & Prevention. Hand Hygiene in Healthcare Settings. https://www.cdc.gov/handhygiene/index.html [Accessed: 12 Jan 2017] World Health Organisation. Five Moments for Hand Hygiene. http://www.who.int/gpsc/tools/Five_moments/en/. [Accessed: 05 Jan 2017] World Health Organisation. SAVE LIVES: Clean Your Hands. http://www.who.int/gpsc/5may/en/. [Accessed: 07 Jan 2017] References
- Jump up↑ Catherine C. Goodman, MBA, PT, CBP and Kenda S. Fuller, PT, NCS. Pathology, 3rd EditionfckLRImplications for the Physical Therapist. Chapter 7 Immune System. pg. 258
- ↑ Jump up to:2.0 2.1 2.2 2.3 HIV/AIDS. Mayo Clinic. http://www.mayoclinic.org/diseases-conditions/hiv-aids/basics/symptoms/con-20013732. Accessed March 25, 2014.
- ↑ Jump up to:3.0 3.1 3.2 3.3 3.4 3.5 3.6 U.S. Department of Health and Human Services. HIV/AIDS Basics. AIDS.gov. http://aids.gov/hiv-aids-basics/. Accessed March 25, 2014.
- ↑ Jump up to:4.0 4.1 Fact sheet 2019 – Latest statistics on the status of the AIDS epidemic | UNAIDS. www.unaids.org.. Last accessed 23 November 2019
- ↑ Jump up to:5.0 5.1 5.2 5.3 5.4 5.5 HIV/AIDS. Center for Disease Control and Prevention. http://www.cdc.gov/hiv/default.html. Updated November 22, 2019. Accessed 23 November 2019.
- ↑ Jump up to:6.0 6.1 6.2 Goodman C, Snyder T. Screening for Immunologic Disease. Differential Diagnosis for Physical Therapists Screening for Referral. 5th Edition. St. Louis, MO: Elsevier Saunders; 2013: 454-457.
- ↑ Jump up to:7.0 7.1 7.2 Goodman C, Fuller K. The Immune System. Pathology Implications for the Physical Therapist. 3rd Edition. St. Louis, MO: Elsevier Saunders; 2009: 257-274.
- ↑ Jump up to:8.0 8.1 8.2 Gazzola L, Tincati C, Monforte AD. Noninfectious HIV-related Comorbidities and HAART Toxicities: Choosing Alternative Antiretroviral Strategies. HIV Therapy; 2010; 4(5): 553-565. Available from: Medscape.com. Accessed March 20, 2014.
- Jump up↑ Treatment for HIV & AIDS. AIDS MEDS: Your Ultimate Guide to HIV Care. http://www.aidsmeds.com/list.shtml. Updated November 18, 2013. Accessed March 25, 2014.
- Jump up↑ El-Sadr, WM; Lundgren, JD; Neaton, JD; Gordin, F; Abrams, D; Arduino, RC; Babiker, A; Burman, W; Clumeck, N; Cohen, CJ; Cohn, D; Cooper, D; Darbyshire, J; Emery, S; Fatkenheuer, G; Gazzard, B; Grund, B; Hoy, J; Klingman, K; Losso, M; Mejia, JMR; Markowitz, N; Neuhaus, J; Phillips, A; Rappoport, C; Strategies Management Antiretrovir,; CD4 count-guided interruption of antiretroviral treatment. NEW ENGL J MED, 2006; 355 (22): 2283 - 2296. http://eprints.ucl.ac.uk/6514/. Accessed March 25, 2014.
- Jump up↑ deBoer H, Cudd S, Andrews M, Leung E, Petrie A, Carusone SC, O’Brien KK. Recommendations for integrating physiotherapy into an interprofessional outpatient care setting for people living with HIV: a qualitative study. BMJ open. 2019 May 1;9(5):e026827.
- ↑ Jump up to:12.0 12.1 O'Brien K, Nixon S, Tynan AM, Glazier R. Aerobic exercise interventions for adults living with HIV/AIDS. Cochrane Database Syst Rev. 2010;(8):CD001796. http://www.ncbi.nlm.nih.gov/pubmed/20687068. Accessed March 25, 2014.
- ↑ Jump up to:13.0 13.1 O'Brien K, Tynan AM, Nixon S, Glazier RH. Effects of progressive resistive exercise in adults living with HIV/AIDS: systematic review and meta-analysis of randomized trials. AIDS Care. 2008; 20:631-653. http://www.ncbi.nlm.nih.gov/pubmed/18576165. Accessed March 25, 2014.
- ↑ Jump up to:14.0 14.1 14.2 Hand G, Phillips K, Dudgeon W, Lyerly G, Durstine J, Burgess S. Moderate intensity exercise training reverses functional aerobic impairment in HIV-infected individuals. AIDS Care. 2008; 20 (9): 1066-1074. http://www.tandfonline.com/doi/abs/10.1080/09540120701796900#.UzGcZNnO_To. Accessed March 25, 2014.
- Jump up↑ Barroso J, Voss J. Fatigue in HIV and AIDS: An Analysis of Evidence. Journal of the Assosciation of Nurses in AIDS Care. January/February 2013; 24: S5-S14. http://www.sciencedirect.com/science/article/pii/S1055329012002427. Accessed March 25, 2014.
- Jump up↑ Bennett N, Bronze M. HIV Disease Differential Diagnoses. Medscape. http://emedicine.medscape.com/article/211316-differential. Updated March 20, 2014. Accessed March 25, 2014.
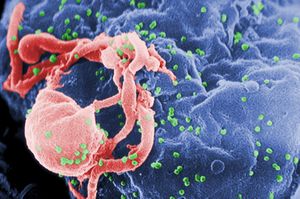
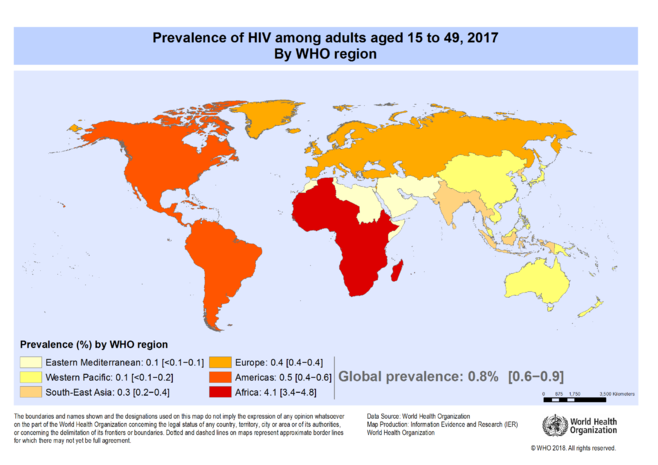
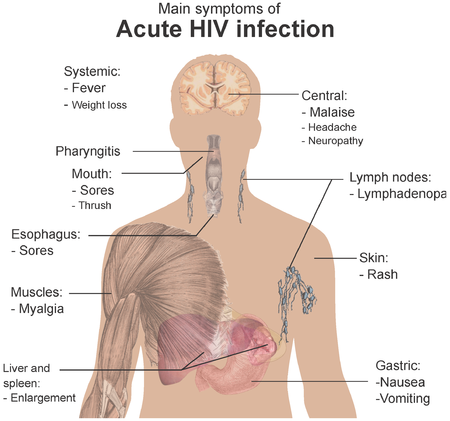
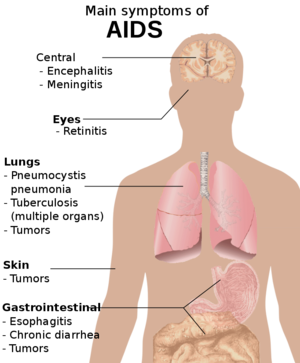









No comments:
Post a Comment